I’ve reached a new physical low and I don’t have any idea of the best direction to go from here. When it comes to my health, I don’t do well emotionally without a plan of action. I can only rest easy when I have prepared for all eventualities to the best of my ability, whether it is going for a drive in the car or thinking about major surgery. As an example, I made a will when I was 37 and, in 2011, I asked my boyfriend of 13 years to marry me so he could legally speak for me if I couldn’t speak for myself. That’s a romantic proposal.
But I’m currently blinded by pain, fear and exhaustion from constant interrupted sleep. I’ve been working so hard this past year to get the appropriate testing of my GI tract, do the hail mary treatments and line up willing surgeons for the operation that is undoubtedly needed, but… a decade into this shite, I am finally at that stage where doctors look at my records and show me the door.
One doctor said right off the bat: “Do you know what scares surgeons the most? EDS [Ehlers-Danlos Syndrome]. Do you know what scares us the second most? MCAS [Mast Cell Activation Syndrome].” She sent me on my way, unwilling to even discuss what was happening anatomically.
I had another surgeon walk into the exam room and, without any greeting whatsoever and without even looking at me, she said, “Well, you certainly are obsessed with your bowels, aren’t you?” Immediately after that, she asked for the name of my therapist. There was more and worse derogatory interactions with her, but I’d like to not get riled up tonight. My great therapist said, “You encountered one of life’s assholes, this one just happened to be a doctor.”
I’ve decided any surgeon who is a) compassionate and b) willing to help people with connective tissue disorders and idiopathic anaphylactic reactions is a bloody hero. I had no idea I would become a medical pariah.
There was a time when I was trying to fix my immune deficiency, my hypotension, my hypothyroidism, my chronic migraines, flu-like symptoms, reactivity etc… It’s all still there and I’d give anything to “just” be dealing with those. I’d have some semblance of life; I’d not be in crisis every day. Sick, yes, but not crisis. I was once chronically, predictably, stably ill and it feels a bit perverse to long for that life again.
Five years ago, I started to have intermittent pelvic floor spasms. Some were very obviously bowel spasms and some were the muscles/ligaments of the entire pelvic floor. The latter were more severe and often triggered a vasovagal collapse where my blood pressure and heart rate would plummet and my husband would call the paramedics. I stopped a lot of things to try to control these. I stopped having periods, I stopped taking stimulant laxatives, I stopped holding my pee, I stopped eating “FODMAP” foods that can generate gas, I stopped having sex.
A year ago, the spasms started to escalate. I had one single episode in January, 2022 and, this week, I have had at least one a day, six days in a row. They are SEVERE. I never use that word lightly. They are agony and I never know how long they will last and whether they will trigger a cascade into hemodynamic instability or loss of consciousness.
The spasms usually start in the mornings when I stand up (or sometimes just sit up in bed) and my intestines drop towards the ground, along with my bladder and uterus (which have also fallen from their normal positions). The weight and pressure this causes on my pelvic floor kicks off a spasm and it is greatly exacerbated by stool or gas in my colon, so eating anything has become scary. Terrifying, actually. Even drinking causes problems — I recently realised that my electrolyte water (TriOral rehydration solution), which I’ve been drinking day and night for two years, was causing a lot of gas production.
Gas causes more issues than anything because it gets trapped in the folds and herniations and the pressure increases to unbearable levels. The pain is blinding. And by “gas,” I really mean air because there is absolutely no smell at all. It is as if someone inserted a hose into my transverse colon and pumped it up. I’ve been eating a very limited diet for years – there really is nothing more I can cut out to try to manage gas production. It’s there even if I fast and it’s made worse by the medications I have to take for constipation like Miralax, Linzess and magnesium oxide. It’s there because I probably have SIBO, too (small intestinal bacterial overgrowth — I’ve treated it many times, but I’m not sure if it’s worked).
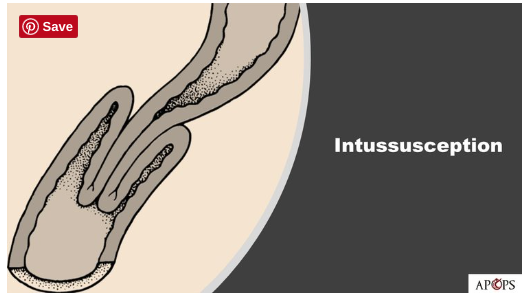
My small bowel is “lying on the bottom of your pelvic floor, like a hose curled in the bottom of a bucket,” one surgeon told me. “Nothing is connected to the sacrum anymore — you have complete internal rectal prolapse with intussusception of the rectosigmoid.” He drew a picture of this “intussusception” – the intestine looks like a sleeve telescoping into itself when you pull your arm out.
My umbrella diagnosis is visceroptosis – abdominal organs falling and prolapsing out of their normal positions – but there are different names depending on which organ has the issue. The ones I have are:
Enterocele: where the small intestine falls between the vaginal wall and rectum (which should be fused, but, in my case, are separated).
Sigmoidocele: essentially the same as an enterocele, only the sigmoid colon has dropped.
Rectocele: the rectum herniates forward and into the vaginal wall.
Cystocele: bladder falls.
Uterine prolapse: uterus falls.
Perineal descent: perineum bulges downward.
Intussusception: telescoping intestine.

The two most profound issues I have on the MRIs are the enterocele and rectocele, above. So, as you can imagine, with both of those bagged-out intestines holding onto poop and gas, prolapsed into the same low-down space, as well as my uterus and bladder sagging, it is an unbelievable amount of pressure on my pelvic floor. The only thing that has helped marginally is lying on an adjustable bed with my head as low as possible and my legs elevated, which allows gravity to shift my intestines back towards my chest. I do this over and over throughout the day to reverse the downward pull – after standing in the kitchen, after sitting at the table or on the toilet. But it doesn’t last long and just moves the pressure under my diaphragm.
Recently, though, things have escalated. Cramps wake me up all night long and, during the day, I can hardly be upright without my pelvic floor going into a spasm. I quickly get on the floor, put cushions under my bum and moan, pant, cry, try to focus all of my attention on relaxing those muscles and easing the weight on the ligaments, while begging the universe to make it stop and vowing to never let anything pass my lips again. I’m hungry all the time.
I can’t keep doing this every day. I don’t want surgery, but I can’t avoid it. I don’t want mesh implanted in my abdomen (my immunologist says absolutely no mesh in someone with a mast cell disease), but I’m told the only other option is a colostomy bag. I’m told whatever I do will probably fail (even the bag) because I will still have slow-transit constipation and shitty connective tissue. I’m told that the spasms might not stop. That thought is very overwhelming. The spasms are more life-altering that anything else. What would the future look like trying to avoid them? Pooping into a bag, but nil by mouth? IV hydration and parenteral nutrition? I need doctors to think outside the box about how to stop the symptom escalation. Botox? Prolotherapy? Nerve stimulators? Nerve blocks? Am I going to have to live mostly on my back to stop my organs from falling?
There are Facebook support groups for everything you can think of, but not for visceroptosis caused by EDS. I’ve met two people in a similar boat. (One of them shared photos of herself in the morning and at night showing how her displaced intestines caused her abdomen to balloon out over the course of the day. I did the same thing yesterday and it is striking, but, although I share everything about myself here, I’m not sure I want to post photos of myself in my knickers. Sorry to disappoint.)
There are no doctors who really understand this particular problem and there is an incredible paucity of studies. A prolapse specialist said to me: “I wouldn’t refer you to any of the colorectal surgeons I know. They really only do routine tumor excisions or coloectomies for things like bowel cancer.”
Oh. I see. What an education I’m getting! Silly me thought that any colorectal surgeon could fix this. My problems are “higher up,” not a “simple” rectocele repair. My issues are from connective tissue laxity, not from pregnancy trauma. Not only do most colorectal surgeons not have the expertise and experience, most wouldn’t take me on, anyway, because they and their hospitals like success – they don’t want to take chances on patients with high rates of complications and surgical failures. These are uncharted waters.
My only plan of action right now is:
- continue doing everything I can to get calories in and out.
- keep trying and retrying bowel medications.
- continue pelvic floor physical therapy (which feels useless – breathing exercises, bowel massages, visualisation).
- get a “small bowel follow through” study (which is proving to be complicated – shocker! – because they don’t usually do upright x-rays and they don’t have any barium drinks that look okay for me to ingest).
- get a mesenteric CT angiogram (which I’ve been putting off for a few years because I had a small reaction to the IV contrast last time and I’m nervous it’ll be a bigger reaction this time).
- talk to my surgeon about a stoma (for a colostomy bag) since he won’t entertain the notion of a repair surgery without mesh.
- trial a fentanyl patch in-office with my immunologist and then other medications to develop a post-op painkiller plan (how on earth do I get the nerve to do this??).
- do I continue looking for other surgeons who have experience with these more complicated, “higher up” repairs and who won’t use mesh?? It’s exhausting and I really don’t think that doctor exists.
But none of that feels possible when I’m so depleted. My husband had a total knee replacement surgery a few weeks ago and the extra walking, driving and chores I was doing made it very evident that my tethered spinal cord is a major player, even though I don’t want to face it. When I’m pushed outside of my energy envelope and normal step count, I have great difficulty walking. I’m hoping now that he has turned a corner with his recovery, I’ll be able to gain some ground and see a clearer path forward.




Big, big hugs for everything you are going through/have gone through. You must be exhausted from the emotional strain alone, let alone the physical pain and lack of sleep and food.
I did wonder if you’d spoken to anyone at the EDS charities, eg EDS society https://www.ehlers-danlos.com/ Surely they must know of surgeons/consultants who treat severe EDS complications?
x
LikeLike
It breaks my heart to read this. You have already been through so much. I wish I had some brilliant insights or secret tips to share, but unfortunately all I can do is send you the biggest, gentlest hugs and let you know I’m thinking about you.
LikeLike