I want to talk about my success with IVIG (intravenous immune globulin) since this is something that I am frequently asked about by other patients. I’m in a very unusual situation where I administer my own IVIG and fluids through peripheral venous lines (not using a port or PICC) at home without a nurse. I feel extraordinarily fortunate to have been able to get this treatment at all, but it feels particularly fortifying during this pandemic. Not only because I am receiving a protective, difficult-to-access medication, but also because, when covid hit, I was in a position to continue treatment uninterrupted in my home without needing nursing visits that would increase my risk of exposure to the virus.
It’s also unusual that my IVIG is prescribed by a naturopath, rather than an MD (let alone an immunologist), and that I do infusions once a week rather than every 3 or 4 weeks, and that I was approved for a high ‘immunomodulatory’ dose without having one of the autoimmune diagnoses that is typically needed and without having to do a vaccine challenge. Also, I don’t have side effects from IVIG, which I find miraculous, but I think it is because of how careful (and controlling) I’ve been throughout the whole journey. I researched and advocated for myself at every turn — undoubtedly more than was really needed — but I have no regrets since it has been such a godsend and I’ve had no bad reactions.
The story starts when I went to see Dr. Chia in 2014 (almost 3 years after getting sick) and he ran a bunch of blood tests that no other doctor had bothered to explore up until that point, such as HHV6 and Coxsackie antibodies, T-cell counts, and total IgG with subclasses.
For anyone navigating the newly-sick morass, I want to point out that I had seen over 30 doctors in those first 3 years, trying desperately to find one big brain that might have some insight. Infectious disease, endocrinology, neurology, allergy, cardiology, rheumatology, sleep doctors, ENT, gastroenterology, functional medicine MDs — you are shunted from one specialty to another to another with no one willing to dig deeper. I am even including appointments with my OBGYN, ophthalmologist and acupuncturist in that count because I was chasing down every lead I could (maybe it’s all hormonal, maybe my eye pain will lead to a brain discovery, maybe ‘dark yin’ is my problem after all). The big issues were missed until I was able to see Dr. Chia and Dr. Kaufman (ME/cfs specialists in California) and — this is the part for anyone who might be overwhelmed with where to start — a local naturopath (ND). In fact, the best help I got in Seattle was from two different NDs: they thought outside of the box and dug a little deeper, like the specialists. And I don’t mean woowoo shit, I mean things like checking for an immune deficiency DUH since I keep telling you it feels like my immune system just broke one day. Soon after I traveled to California to see Dr. Chia, I found an ND who ran almost the same battery of tests which revealed the same abnormal results. The first ND, who agreed I needed IVIG, but couldn’t get it for me, tried a bag of different tricks aimed at increasing my IgG levels. They didn’t work, but I was very grateful to have someone try something. Point being, if you can’t see a specialist, I would advise finding an ND who will look at your immune system health and infections and who is willing to walk the long road with you, being patient while you try (and, in my case, most often fail) different treatments.
But, I got ahead of myself. Dr. Chia saw that my total IgG was low and so were some of the IgG subclasses. He said I needed IVIG, but he didn’t offer to get it for me (I thought at the time it was because he was in California, but I now know Seattle patients that get IVIG through Cali doctors, so I’m not sure why he couldn’t have ordered it). Once I was back home, I asked my 4 doctors if they could help me get IVIG (primary care doctor, rheumatologist, endocrinologist, ND) and they all said no. My PCP did go a little further by asking an immunologist colleague, but he said my IgG would need to be lower or I’d have to do a vaccine challenge, which I refused.
I had given up and stopped asking when I found my second ND (who was very different from my first; both have been helpful in separate ways). The very first thing she said after entering the room on our first meeting was: “You need IVIG.” She had reviewed my lab work (she had reviewed my lab work!! I don’t think any other doctors had actually looked at anything ahead of time) and seen that my IgG was continuing to decrease over the months. I had hypogammaglobulinemia and fit the diagnosis for common variable immune deficiency (CVID) and she was confident insurance would approve immune globulin therapy.
Between that day and my first infusion, 11 months went by. I delayed until I felt I had thoroughly prepared in every way to keep myself safe. Anaphylactic or anaphylactoid reactions can occur in any patient receiving IVIG therapy, but I had a history of both (plus intractable migraines), so I was nervous and wanted to control every aspect of treatment. My doctor was patient and accommodating. I don’t think any other doctor would have let me take the time to tackle each concern and build up the confidence to take the plunge. I think of it a little like a lost year when I could have been feeling better, but, like I said, I really can’t have regrets when things went so well.
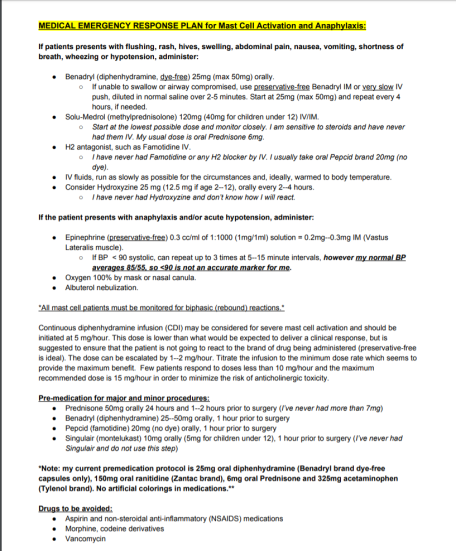
First off was figuring out how to safely take pre-medications for potential reactions to the immunoglobulin and how to get IV fluids (which would be administered before IVIG) without side effects. I was extremely reactive back then because of out-of-control mast cells and I had no safe rescue medications or pre-medication protocol. IV fluids had caused angioedema and breathing issues; I was so sensitive to Benadryl, I couldn’t even take drops without feeling anticholinergic-type symptoms; tiny crumbs of steroids made me feel like was hit by a truck, running on a treadmill and sedated all at once. I didn’t feel comfortable doing IVIG without having a rescue protocol, so, during that year, I worked on my tolerance and put together a safe plan.
First, my doctor put me on bioidentical hormones because there is some evidence that they can help with mast cell reactivity. Then, we tried IV fluids, but only 250 mls, warmed up and run at a snail’s pace (my previous reactions were from 2,000 mls of cold fluids run very quickly on the day my period was due (when I’m highly reactive); I didn’t know any better). I even found out I was fine with two types of normal saline bags, but not another. I slowly gained tolerance to Benadryl (dye-free capsules, only) and Prednisone (finding manufacturers with the cleanest excipients), taking bigger and bigger slivers until I knew I could safely premedicate before infusions. Those that know me understand that the symptoms that have scarred me the most are my mast cell reactions. They are unpredictable and violent. Full-blown anaphylaxis almost killed me. I can’t adequately express how jubilant I was to have a safety net, to have protection, to be able to put a protocol on paper that anybody could follow in case of an emergency and to have tools with which to arm myself before a procedure. Having intolerable side effects from the things that are meant to counteract intolerable side effects was a scary place to be.
Next, I talked to my doctor about starting with subcutaneous infusions (SCIG), rather than intravenous because all of my research indicated that the former was safer. She agreed, thankfully, although she gently pushed for IV for years after that. I also asked if I could start with 1 gram at a very slow rate of delivery and she acquiesced to that, too. NO allopathic immunologist would have agreed to that EVER.
Then I looked into a hospital infusion versus an ambulatory infusion suite (AIS) versus at-home infusions. I was told a hospital wasn’t an option and the AIS was staffed only with a nurse, no physician. If I had a reaction, the protocol was for the nurse to administer supportive meds and call 911, if needed. Well, staying at home was a no-brainer. I would have a nurse in my house, but, more importantly, I feel much safer with my husband there as an advocate. Plus, we live very close to an emergency room and he could whisk me there if calling an ambulance didn’t feel like the appropriate move. In the past, we have sat in our car in the ER parking lot, waiting to see how reactions progressed. The high price of healthcare in this country is a great deterrent.
Then I wanted to look into IgA deficiency. There is some research that low serum IgA and anti-IgA antibodies increase the risk of anaphylaxis and the remedy would be to use a very low-IgA brand of immune globulin for my infusion (says my Labcorp test result: “Patients with IgG antibodies against IgA may suffer from anaphylactoid reactions when given IVIG that contains small quantities of IgA. In one study (Clinical Immunology 2007;122:156) five out of eight patients with IgG anti-IgA antibodies developed anaphylactoid reactions when IVIG was administered.”). My total IgA and one IgA subclass had been low in the past, but neither my doctor nor the infusion pharmacist suggested that this should be a consideration — I had to get the info from other patients and insist (nicely) that we test my anti-IgA antibodies. Gamunex-C was the brand that had already been approved by insurance and I knew that I was very lucky to have it and might lose it if we had to resubmit an authorisation, but safety first. Gammagard could have been a safer choice since it has extremely low IgA content. It took an excruciatingly long time to get those results but, ultimately, I did not show anti-IgA antibodies, so we pressed ahead with Gamunex. And I’m glad we did! One of my nurses commented that it is the “top shelf” immune globulin and it’s been good to me.
The final hurdle was scheduling. Back then, I was much sicker in the mornings — shaky and very low blood pressure — but that is the time of day when nurses typically arrive for long appointments. I always thought, if I became a home infusion nurse, I would offer nights and weekends, just like my preferred shifts in the restaurants. There must be more patients like I am whose vitals stabilize as the day goes on. Also, my period was looming, a time of the month when I am highly reactive, so I wanted to avoid that whole week (although this wasn’t as easy as it sounds because my cycle wasn’t/isn’t regular). The day came when things eventually fell into place and my wonderful nurse, Marie, came to my house to hook up the IV fluids and teach me how to infuse subcutaneously. She showered beforehand and changed her clothes because she and some of her other patients have cats. She understood my nervousness and didn’t rush me or complain even though she had to sit in one room with me in a straight-backed chair for 8 hours. Marie came every week for 16 months to hook up my IV, but, once we knew I was doing well on this treatment, she was able to leave quickly and I would disconnect my IV fluids and do the SCIG myself.

We started with 1 gram infused through a 2-needle set and F30 tubing. That probably made anyone knowledgeable with immunoglobulin infusions laugh because it is SO SLOW. Like, unheard of. My nurse had to do a special order for the supplies because they are normally only used for infants. Over the weeks, we slowly worked up to 5 grams (eventually using a 3-needle set and F45 tubing — only slightly faster), which is a typical ‘replacement’ dose for a primary immune deficiency patient of my weight. I stayed there for a year and a half, not pushing my luck in any way. Slow and steady.
In 2017, a miracle: I switched infusion companies from Coram to Accredo (with nothing to which to compare Coram, I thought they were fine, but things have been much better with Accredo) and they suggested I learn to insert my own IV catheter for fluids. Uuh, yes, please! Actually, they suggested my husband do it, but he’s not good at these things and I am, so a nurse came over and gave me a tutorial and that was that. I was only “allowed” one training session, so I wound up watching a ton of YouTube videos, which is why I’ve now made my own, in case they can be helpful for anyone.
For over 3 years, I’ve been placing my own peripheral IVs each week. It gets easier and easier and, honestly, I feel so much safer. Although Marie was very careful, I am more careful because I have a bigger stake in the game. I do not want to ruin any veins or get an infection, so I am vigilant (and superstitious) about my aseptic technique and I rotate veins to give them a break. Every single week, for the entire 16 months that Marie was my nurse, she used the left median cubital vein (antecubital or, as my nurses called it, the “AC vein”). I never questioned it because it held up well, but that’s about 60 catheters inserted in the same place (what a trooper my vein was!). As soon as I was doing it myself (and discovered I was ambidextrous when it comes to IV placement), I started using a different vein each week. I have 6 sites that I use, but 2 of them (on the outside of my forearms) are difficult — the veins roll and there’s always more of a risk of having to do multiple pokes — so I use the cephalic and AC veins more often than not, even though it means having to keep my arm straighter. I don’t use my hands or wrists, partly because I wash my hands so often, it’s an inconvenience and partly because I want to save those sites for easy access if I’m ever in the hospital with a nurse that needs fat veins for larger gauge needles.

Holy roller
Then in 2018, another miracle: I switched from SCIG to IVIG and was able to continue to do it myself at home. Not only that, but I was allowed to continue infusing once a week, which kept my levels more consistent with fewer peaks and troughs, which in turn kept my energy more stable. IVIG is typically given every 3 or 4 weeks for multiple days in a row, necessitating a peripheral IV be left in place for 3 or 4 days (I can’t even imagine; 12 hours feels like an eternity). This is one of the reasons so many people get PICCs or ports.
I am regularly asked how I managed to get self-infusion approved at home. I didn’t do anything. I didn’t even know it was something that was allowed. I lucked into it with a good doctor, a good infusion company and a good nurse.
The first year I was with Accredo, I had increased my SCIG dose from 5 grams to 10 grams. My legs (my preferred place for the subcutaneous needles) weren’t happy, though. They weren’t absorbing the medication as well as they used to and they were swollen and sore for longer afterwards. I was using 6-needle sets to try to stop leaking and I felt like a pin cushion. I also wanted the option of trying high-dose IgG (my specialist had said for years that I needed 20 grams/week) in the remote chance that insurance would approve it. So I talked to my doctor about changing brands to one with a higher concentration, which would mean less fluid infused into my tissue. I was still adamant that I didn’t want to try IVIG. I didn’t want to tempt fate and I was scared of medications going directly into my veins and causing an instant reaction. My doctor pointed out that my body liked Gamunex, so I could either stick with what we knew didn’t cause a reaction (because Gamunex can be infused by either route) or stick with SCIG and change brands. I decided that it felt safer to stick with the brand I knew and loved, so IVIG it was.
They sent a home health nurse to do the first IVIG infusion. I had already placed my IV catheter and run my fluids when she arrived and she said it was perfect. Once again, we started at a low dose (2.5 grams) and ran it very slowly. We worked back up to 10 grams a week over a few months. During this time, I changed from the first awful, bullying nurse to one I adored (we could be friends in a different life). Jennifer showed me how to run the IVIG after the fluids and made sure I did everything right, but one week she said, “I’m just a fly on the wall. You place the IV, you run the fluids and medication, you disconnect. There’s no point in my being here.” So she recommended to my doctor that I do it alone under the condition that I have a responsible adult available at all times during an infusion in the case of anaphylaxis. That’s how I wound up doing it without a nurse and I’ve never met anyone else who is in this same situation.
The final miracle happened this year: My insurance approved the high dose IVIG (20 grams a week, which works out to almost 2g/kg/month, what is considered autoimmune or immunomodulatory dosing). I’m not sure which of my ridiculously high titers got it authorised and I’m not going to question it, I just thank the universe each week and try to keep finding the money (my 20% copay is $1,400/month). I increased slowly over months and had some headaches in the beginning, but nothing now. I am energised the day after. It’s like liquid life-force. I only premedicate with 25mg Benadryl, 20mg Pepcid and 4mg of Prednisone and I could probably do less. The number one benefit to doing it solo is that I’m able to program the flow rate as slowly as I like, which ameliorates side effects. If I had medical oversight, I’m sure they would insist I increase the rate, if for no other reason than to get the nurse out of here quicker. Talking to friends who have dealt with aseptic meningitis or incapacitating migraines, it seems to me that flow rate being too high is the major precipitating factor.
IVIG changed my life. I started the first wee tiny dose on October 2nd, 2015 and improvements in ME symptoms happened very quickly. By January 2016, I felt confident enough to write about them. They marked the end of 4 years of a steep and terrifying downhill trajectory and the beginning of a very slow, but steady uphill trajectory for the past 5 years. There have been lots of setbacks, plateaus and crashes (scary ones and months-long), but, overall, I’m stronger and more able-bodied each year over the last.
There are so many things I’ve learned along the way that I want to share like: try to get shelf-stable bags of fluids. My first pharmacy removed the air from the bags of saline before sending them and I didn’t know that there was another option. Once the bags have been accessed to remove air, they have to be refrigerated and thrown out after 14 days. They take up a lot of room in the fridge, it take ages for them to come to room (or body) temperature and you can’t have extras on hand when they’re considered unsafe after a few weeks. My bags now can be stored at room temperature in my closet and their expiration dates are years away, which means I have them for emergencies and don’t need to go to the hospital if all I think they can do for me is administer fluids (which is what has happened so many times in the past with my vasovagal collapses).
This took on even greater importance when covid hit. I feel so lucky to have extra supplies and the ability to give myself IV fluids without going near healthcare facilities. When I’m doing the clean-out for an upcoming colonoscopy, my doctor wants me to give myself IV fluids, which I wouldn’t have been able to do without this lucky situation. And when I imagine the big earthquake or an end-of-world emergency, it gives me solace to know that I am trained and my home is so well equipped.
I’ve also learned that I never want to use gravity tubing and an IV pole when a pump and carrier bag is so much easier, safer and more precise. I don’t have to keep my fluids vertical and elevated, dragging a pole around the house; I can walk around with the bag holding the saline and pump on my shoulder like a purse. I’ve even gone to doctor appointments and run fluids in the car during our California road trip last year after a big blood draw.
I learned from other patients to prime the air out of the bags through the tubing before priming the saline (fill the tubing with saline), which seemed slightly safer than the way a nurse showed me using a syringe, which requires accessing the rubber stopper. Uses fewer supplies, too. Less plastic waste.

Medical waste
I called B. Braun, the company that makes my normal saline, and learned how to safely warm the bags before administration, so I don’t react to the room temperature (which is chilly!) fluids. I figured out that running fluids at a slower rate (150ml/hour) cut down on post-infusion headaches and it was even more effective to bookend the Gamunex with 500ml of saline before and after, rather than running the entire liter beforehand.
I learned that I can keep using the pump for 12 hours after it beeps that the battery is low. Again, less waste. (Although, I wouldn’t sleep with a low battery, just in case.) And I learned that the Bodyguard pump’s beeps terrified my dogs because they were too similar to our fire detector, but the CADD Prism’s beeps go unnoticed.

Bad beeper
Wonderful nurse Jennifer gave me a fabric one-handed tourniquet which has made such a difference to my independence and the comfort of my skin. She also taught me that if the ultrasite on the saline lock is going to be unattached for any length of time and I don’t have a cap for it, an old nursing trick is to stick it inside an alcohol prep pad (leaving the wrapper on) and secure it with tape.
Wonderful nurse Marie taught me how to use gauze to support the catheter if it doesn’t lie flush with the skin and how to tape a loop of tubing to your arm, which has stopped my IV from being yanked out many times when I snag it on something. She also always used alcohol prep pads and iodine to clean the insertion site, something which many find overkill, but makes me feel more confident in my infection control.
I learned the catheters with wings are much easier for me to insert than the ones without and that you can ask for sterile gloves rather than relying on the box of non-sterile gloves that they send by default. I learned that you can order sterile pads on which to lay your supplies and IV3000 adhesive dressing that doesn’t tear up your skin like the Tegaderm that comes inside IV start kits.
I figured out by trial and error that some veins need to be stretched taut and stabilised and, if you are inserting your own IV and don’t have two hands, there are ways to do this by twisting your forearm and flexing your hand. I also found out that some veins are close to nerves and your thumb might have pins and needles for weeks afterwards, but they will, thankfully, eventually go away.
During SCIG, I learned that there are handy rate and time calculators for subcutaneous infusions and that if you are having trouble with leaking, swelling, hitting blood vessels etc., that you can try different needle lengths and different needle brands and — the key for me for whatever reason — different needle tops (the soft adhesive ones worked best for me rather than the hard plastic ones that needed to be covered with Tegaderm). I also learned that fat is key to comfort — the medication was much better absorbed if I put the needles in the back of my hips/ top of my butt (saddlebags??).
The most important thing I’ve learned is that although most patients in online support groups ARE NOT MEDICAL PROFESSIONALS AND YOU SHOULD ALWAYS CONSULT YOUR DOCTOR ABOUT EVERYTHING, they are a wealth of information. Doctors and pharmacies didn’t tell me anything about how to manage infusions safely. The majority of my home health care nurses didn’t verbally educate me — it was up to me to observe, ask questions and do my research.









