13 months after my California doctor wrote the prescriptions for two gut antibiotics to treat SIBO, today is the day I have to face the music. I’ve put it off for this long out of fear: Fear of a mast cell reaction (Rifaximin ingredients: Sunset Yellow FCF, ffs); fear of no reaction, but feeling terrible from die-off (we just arrived in the Cali desert for a month, so it’s really fear of destroying my idyllic get-away); fear of altering my microbiome for the worse, rather than the better (causing more of a candida flare, causing C. diff etc); fear of spending the money, but not not being able to take the medicine (each one was $200!). Also, although the SIBO test was “off the charts” (in my doctor’s words), I don’t have the symptoms, so fear of messing with the gut I know and creating new issues. I haven’t taken an antibiotic in almost a decade–well before I got sick–so, there’s fear there, too.

But I see my doctor later this month and I’m determined to do the treatment before I see him. I now have both medications in front of me, money is spent, no excuses. One of them is compounded in sterile water and needs to be thrown out in a few weeks, so I’m starting now, with one drop, as soon as I stop typing… which, of course, makes me want to keep typing, keep putting it off, what else can I tell you…?
_
_
_
Okay, I’ll quickly tell you a good drug story, which will bolster my confidence. The first medication I was ever prescribed after getting sick was hydrocortisone. The pharmacist said, “If it gives you a headache, let me know.” It gave me a whopping headache and, back then, I didn’t understand my reactions and how I have to start at micro-doses–I didn’t even know you could cut a tablet or open a capsule–so, I just stopped taking it after two days. The ND said she presented my case to her colleagues and everyone said, “Yes, hydrocortisone!” but it was my first experience with an ND and perhaps I didn’t fully trust her, but, more so, I didn’t want any worsening symptoms, so I just stopped going to her. That has been my MO thus far: try not to rock the boat, except very gently, over a very long period of time (and, by the way, for the most part, I have improved over the years (knock on wood, toba, toba), which has reinforced my careful tendencies).
Last year, my California MD Rxed hydrocortisone again. I tried an 1/8 of a tablet in August and felt short of breath, so didn’t take it again until 3 months later. Then I was spurred on by a receptionist at a doctor’s office who started crying (!) on the phone to me while talking about her daughter who needs hydrocortisone all day long, so I tried it again. It went okay for a few months. Then one day it made me feel gittery, spacey and short of breath again. Then, a few weeks after that, it hit me like a freight train. I wrote in my calender: “Shaky, drugged, agitated, buzzy muscles, feel like I’m on speed, then possible blood sugar crash (or maybe just still shakes from hydrocortisone). Then, after hours, a dull obvious-reaction headache and stuffed ears.”
This is what used to happen to me with antihistamines: I’d handle them for days and then, without warning, the same dose would send me into a scary cascade of anticholinergic symptoms (I still mourn the loss of Unisom, which helped a lot with sleep for a while).
But, I persevered with the hydrocortisone (yay, me!) and, last month, something clicked, I could feel it help my body. I can feel the uptick in energy and the decrease in brain symptoms. I give hydrocortisone full credit for getting me through the weeks of packing for this trip and those back-to-back high-step count days. Each morning, I marveled: I’m not bedbound, I think I can do it again. I have no side effects now and I might even try more than a 1/4 tablet. 😉
Grab that cash with both hands and make a stash.
This is a hard one to talk about. It’ll be more of a rant. And I’d like to preface it with all of the obvious about how grateful I am that we were in the economic position we were in when this illness started, how grateful I am that I had a few years of good earnings and decent savings, how grateful I am that my family is healthy and has never been bankrupted by health woes. I am, I truly am, and I think about–probably too much–what must happen to others with a severe chronic illness (that has no knowledgeable doctors and no decent treatment) who are in worse financial shape than we are, without our resources, who are in countries steeped in poverty, refugees fleeing wars… on and on… I do know how lucky I am. But, I’m scared. Mostly because I don’t know what treatment to spend money on and what to reject.
Recently, after 6 months of immunoglobulin infusions, I got a slew of bills that I didn’t anticipate. It turns out that for my itsy bitsy dose of 5 grams each week, I pay $164 after insurance. Out-of-pocket. That’s $655 per month. If I had known this before starting, would I have done it? I don’t know. But now that this is the only treatment that has helped me, how can I stop? And I’m in this tricky spot. I have private health insurance because I was too scared Medicare wouldn’t cover these treatments (also because Medicare won’t cover acupuncture, nutritionists or physical/myofascial/craniosacral/massage therapy — some of the only things that have made a difference in my pain levels). After being told IVIG was not an option by so many doctors, knowing that I didn’t have a history of bacterial infections and a vaccine challenge is usually required for approval, and having Coram (the infusion service) tell me that Medicare hardly ever covers treatment, I was just too scared to give up the private health insurance that had already approved my treatment for the whole year. Of course, I have since heard from others that Medicare covers their IVIG or SCIG at 100%, but … how could I risk changing coverage now when my IgG levels have come up and that alone might disqualify me from continued treatment? I’ll have to revisit this next January when I’m eligible for Medicare enrollment again, but, if I’m still improving with my infusions, I don’t know how I’d take that leap of faith.
An aside for those in other countries or for those that don’t know this fucked up aspect of our healthcare system here in the U.S.: Medicare (government health coverage) isn’t free. You pay each month just as you do with private health insurance. It’s usually cheaper, but not always. It can range from $105-$771 a month, depending on your situation (the higher end is reserved for people who have not worked enough in their lifetimes to qualify. So, if you are struck down with a chronic illness as a young adult and you haven’t worked the requisite 30 quarters in a tax-paying job, you’re not married and you undoubtedly have little savings, then you get to pay the highest premium for our national health coverage– oh, but only if you’re lucky enough to be granted full disability, which very few ME/CFS/Lyme sufferers are). And don’t think that Medicare actually covers your healthcare in full, though. You will still have a deductible each year and co-insurance (the patient pays 20%, typically), you’re prescription medications aren’t paid for unless you get extra coverage and hospital stays can still leave you in horrendous debt. You can stay in a hospital for a few months for the low, low price of $1,260 (although skilled nursing facilities will be more because that price doesn’t cover people to care for you), but let’s take a pretty terrible example: 150 days in the hospital. In 2015, that would have cost you $47,565 out-of-pocket. If you had to stay any longer, all additional costs are your problem. The government washes its hands of you. But wait, there’s more! If you choose not to enroll in Medicare when you become eligible, your monthly payment when you do enroll will be higher–forever–usually 10% higher for each year you could have signed up but didn’t. In my case, if I’m covered by Medicare next year, I will be paying an extra $300/year because I didn’t enroll when I first became eligible. If I wait until 2018, I’ll pay a penalty of at least $440 that year, plus more each year as the premiums continue to rise over my lifetime. Lovely.
SO… Last month I finished up weeks of financial slog for our 2015 taxes and was happy to see our (and by our, I mean my because my husband’s medical expenses are only about a quarter of our total and that is solely health insurance premiums because he never needs a doctor, knock on wood, toba toba) out-of-pocket medical costs had come down slightly.
2012: $14,480
2013: $19,032
2014: $19,564
2015: $17,912
That doesn’t allay the fear, however. After utilities (sewer, water, garbage, recycling, gas, electricity) and mortgage payments, we’re left with about $20K a year to live on and medical expenses have been almost $20K a year since I got sick. That means most everything else–food, clothes, toiletries, dogs, phone, internet, gas for cars– comes out of our savings. I’m trying to be healthier, place fewer burdens on my system and subdue my chemical sensitivities by eating organic food, pastured meat and buying less toxic products. All of these things are more expensive. For the last year and a half, I’ve been paying $200/month for compounded medications instead of the cheap, generic, filler-filled ones. It hardly costs anything to get sick, but the system is rigged to bankrupt those that are.
I feel very fortunate that we had saved money before this happened, but it will run out eventually and I don’t want to make all the wrong decisions now because I’m frozen in fear of the future. Our day-to-day living is all-encompassing, so time slips by in survival mode and the big decisions never get discussed. I’m happy that we didn’t sell the house when I first got sick because we’re finally not under water and it might actually be worth what we owe again. But when do we sell? And do I switch back to generic meds? Do I stop supplements (around $100/month)? Do I stop seeing my doctor who doesn’t take health insurance? Do I not try human growth hormone or hyperbaric oxygen or nutritional IVs? Do I stop my immunoglobulin infusions?? Last year, I thought a time would come when we just moved somewhere very small and affordable, maybe a foreign country, and I stopped all medical visits and we tried to exist on pittance and make our money last as long as possible… But now that I’ve found a treatment that helps my functioning, I have renewed hope. Maybe I’ll be able to earn a living again if I keep making progress. How can I give up on that? Or should I accept the fact that this is as good as it’s going to get, income-wise? My husband will get older, he’ll be able to work his manual-labour job less and less and I won’t ever recover to the point of being able to hold a job… I think that’s the reality. I know a lot of people with this illness and many have made improvements, but I’m not sure if I know any that have gone back to full-time work.
So, we beat on, boats against the current, cut costs where we can, shop the deals online, grow some veggies, sell some stuff, and pray that in ten years time, the tides have changed for the better.
Migraine Help From Headache Neurologist
Last year I was taking an Uber (taxi service) to an appointment and, thankfully, the car wasn’t smelly with cleaning products or dangling air fresheners, but the driver had the radio on and I’ve found background noise difficult since I got sick. I asked him if he would mind turning it down because I had a migraine, which wasn’t exactly true in that moment, but I do get migraines and that’s usually a good excuse for the taxi conversation about scents and noise and why you have your sunglasses on and the window down when it’s gloomy and raining. Turns out, this man had to leave his 9 to 5 job because of crippling migraines and was really suffering until he saw a local neurologist. He said he was having a hard time with migraine meds and she put him on this mitochondrial supplement and a natural regimen that helped tremendously (my ears perked up at a random stranger talking about mitochondrial deficits causing migraines, so I bought the supplement right away, but haven’t gotten around to taking it in the last eight months). Of course, I wrote the specialist’s info down and, when I saw my therapist, I mentioned this doctor to him (my therapist sees lots of people with complex illnesses like mine and has a network of good doctors that he recommends based on feedback from patients). “Oh yes, I’ve heard great things about Dr. Murinova,” said my therapist, so that sealed the deal, I wanted to see her. “But she stopped taking new patients.” Somehow, though, I managed to slip in and get an appointment and, it was true, when I tried to reschedule it, she had nothing else open for the rest of the year, so I felt fortunate (and kept the appointment).
There are some not-so-glowing online reviews of Dr. M, but most seem to center on her brusque demeanor. She’s Eastern European and has that sort of no nonsense approach, which doesn’t bother me at all. I quite like it, in fact. At one point, I told her it would be really difficult to wake up early enough to see the morning sun and she looked at me hard and said, “Do you want to get better or not?” Gulp. Yes, I want to get better! She said there was no point in eating good food and enough protein if you aren’t getting up in the morning because the blue light signals the pineal gland to convert protein to serotonin and melatonin (see her handout below). Her bluntness was effective. I haven’t managed to change my sleep schedule, but I certainly started taking it more seriously.

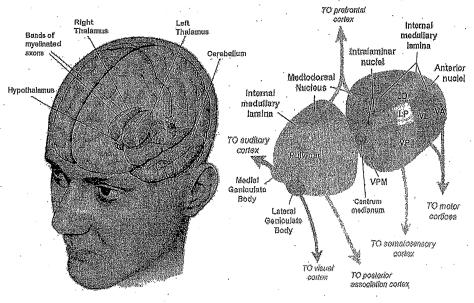 She diagnosed me with: “Chronic intractable migraine, with status migrainosus and occipital neuralgia.” She also gave me a physical exam and then diagnosed me with fibromyalgia before we’d even talked about my primary illness. Believe it or not, that was the first proper hands-on work-up I’ve had for fibromyalgia since being sick — even during those early years of excruciating body pain. She said migraines are tied to mitochondrial insufficiency, IBS, fibromyalgia etc. and that low available energy kicks off the trigeminal nerve alarm which causes pain. My genetic predisposition (my father has a long history of cluster headaches) coupled with central sensitization and not enough energy to power the thalamus properly = migraines. I thought she was very thorough and obviously extremely knowledgeable. I especially liked that she had a natural protocol and a medication protocol depending on patients’ needs.
She diagnosed me with: “Chronic intractable migraine, with status migrainosus and occipital neuralgia.” She also gave me a physical exam and then diagnosed me with fibromyalgia before we’d even talked about my primary illness. Believe it or not, that was the first proper hands-on work-up I’ve had for fibromyalgia since being sick — even during those early years of excruciating body pain. She said migraines are tied to mitochondrial insufficiency, IBS, fibromyalgia etc. and that low available energy kicks off the trigeminal nerve alarm which causes pain. My genetic predisposition (my father has a long history of cluster headaches) coupled with central sensitization and not enough energy to power the thalamus properly = migraines. I thought she was very thorough and obviously extremely knowledgeable. I especially liked that she had a natural protocol and a medication protocol depending on patients’ needs.
Below is the plan she gave me. I can’t say it is definitely her advice that has helped (I started immunoglobulin infusions right after seeing Dr. M), but my headaches have been much better in the last six months.
- Change my posture (shoulders back and scapula close together). She said it will feel unnatural, but bring the shoulder blades together as much as possible. I’ve been doing this.
- Yoga might help neck issues. Haven’t tried this yet.
- Aerobic exercise and build muscle to feed mitochondria. My goal.
- Good nutrition and enough protein. Try ish.
- Deep breathing, relaxation and other parasympathetic nervous system activities. I do these daily.
- Sleep better, but wake yourself up early for outside light from 7-9am to build serotonin (that time is very important for short wave light that feeds your brain; you need it to cross the retinas, but not through a window. She felt this was non-negotiable). I haven’t managed this, of course.
- No more Tylenol (more than one a week will perpetuate headaches). Now I only take it once a week for my immunoglobulin infusions and on the rare occasion of a bad headache.
- Drink up to 3 cups a day of feverfew tea (she thought this was most important. She has weaned patients off migraine meds with this tea). I drink it daily.
- Consider SAMe (200mg/day), yarrow formula, magnesium, coq10, riboflavin (I already take the last three), other B vitamins (B12 shots are a possibility for a boost).
- A device called Cefaly, which works on the trigeminal nerve to break the feedback loop and is proven to greatly reduce migraines. $300 out of Costco in Canada.
- Instead of Tylenol, consider low-dose Lyrica as bridge drug, not a permanent therapy.
- Book: Chronic Pain and Fibromyalgia by Stephen Stahl.
- The study she gave me is great reading. It also suggested acupuncture, oxygen, capsaicin and butterbur, but she didn’t specifically mention those.
- She also gave me the following handout, which you can hopefully enlarge to read:

1
Treatment Update
Today (actually last Thursday, it took me a while to write this), I had my follow-up appointment with Dr. Kim to go over the gaggle of blood tests I had done in March. There is a lot that I am adding into my regimen, so I wanted to document it all asap before I forget everything she said.
We’re going to try hyperbaric oxygen therapy! I said it as a joke as we walked past the room with the claustrophobia chamber: “When do I get to dive?” And she thought it was actually a good idea. So, I’m going to start with a very short time (10-15 minutes) and work up to 60 minutes “at depth”, with supplemental oxygen, once a week. This is out-of-pocket, of course, and pricey at $150-$175 per 60-minute session, so I’ll try a few and see how I do.
I am starting a slow treatment for candida with Nystatin, Diflucan and Thorne SF722. Here’s the protocol:
*Nystatin on Mondays and 2 capsules a day of Thorne SF722 Tuesday through Sunday for 3 weeks.
*Then the same thing with Diflucan on Mondays for 3 weeks.
*Then Nysatin Mondays, Diflucan Thursdays and 2 SF722s on the other days for 2 months.
She didn’t mention diet and I didn’t bring it up. Yippee!
I’m increasing oral progesterone to 100mg/day (I’m at 25mg now), staying at 25mg of oral pregnenolone (uh oh, I just realised while adding this link that I’ve been swallowing my pregnenolone whole, not realising it’s sublingual… grreeaaat 😝) and changing from topical DHEA to 25mg oral.
My sex hormone binding globulin (SHBG) is high, which she said functionally lowers hormone levels. I’m going to start nettle root capsules (work up to 300mg twice a day) to bring SHBG down (not to be confused with nettle leaf, which I drink in tea every day).
I’m not anemic, but my iron is low. She wants me to add Floridix, but after reviewing the ingredients, I may just do a generic ferrous gluconate supplement for 6 months.
For sleep:
*5HTP, 75-150 mg at night (this was recommended by a friend–thank you, M–and Dr. Kim thought it was worth a shot). She says it may even interact with the 5HT4 receptors in my GI tract and help motility. 30-50 mg P5P (active vitamin B6) should be taken with 5HTP.
*Dr. Yasko recommended I get my lithium tested (she answered a quick question on Facebook, I’m not working with her) and Dr. Kim thought I could try supplementing a 20-40 mg per day without a test and see if it helps.
*Belsomra, a prescription sleep medication given to me by my sleep doctor, is still sitting on my shelf a year later and I intend to take a small nibble one of these days. It doesn’t interact with 5HTP, so I can try all the things.
For constipation, I am going to try MotilPro (work up to 3 capsules morning and noon) and a bit of iodine in the form of potassium iodide (5-20 mg 4 times per week).
She said my vitamin D at 40.4 ng/mL is actually fine and I should continue taking 4,000iu/day (I take Thorne liquid D3+K2). She bases this on my calcitriol (vitamin D 1,25) number, which is good at 48.2pg/mL, right in the middle of the range.
She’s not worried about my high cholesterol or LDL at all, so I’m going to shake off my concern about that and trust her.
She said not to worry about an Igenex lyme test or my positive bartonella test for now. She is going to treat my high mycoplasma pneumoniae eventually and she said that treatment is similar to what she’d do for tick-borne infections. I have to say, I kind of like that a reputable LLND isn’t jumping straight into Lyme testing and treatment. She’s definitely not a one-trick pony.
I’ll start antimicrobials for M. pneumoniae, CMV, HHV6 and EBV later this year when my body is stronger. She thinks it will most likely take at least 2 years to get those blood tests into the normal ranges (to the point where my immune system isn’t mounting a response against reactivated infections).
Other supplements* and prescriptions I currently take, many sporadically:
MitoCore
CoQ10/ubiquinol
Humic Acid
Thorne Trace Minerals
Thorne Riboflavin-5-phosphate
Thorne Niacel
Thorne vitamin D3+K2
Thorne B complex #6
Magnesium malate
Magnesium glycinate
Jigsaw magnesium
Potassium gluconate
Biotin
Thiamin
Vitamin A
Vitamin C
Wormwood
HCL + gentian + pepsin
Enzymedica Digest Basic
Enzymedica Digest Spectrum
Charcoal
Levothyroxine (100mcg/day)
Liothyronine (15mcg twice/day)
Prednisone (3mg), Benadryl (25mg), Zantac (10mg), fluids (sodium chloride 0.9%, 1 liter) and Gamunex-C (5g) during infusions.
*By the way, all the supplement links here are for Pure Formulas (and all brands are gluten-free, soy-free and well-regarded). I am not affiliated with them in any way and I can’t get kick-backs if you buy something from these links like lots of bloggers that make money that way (although, maybe I should look into that!). I’ve just done a lot of research and they are consistently the best for me. If you decide to order from them and you want to be a kind and selfless friend, you can use my referral code: RRKMLW or shop here. Once you complete an order (without using any of your own reward points), I get a $10 credit. 😀 I like Pure Formulas because a) free shipping with no minimum; b) 2-day shipping always if you have ShopRunner, which I do through my AmEx; c) you earn cash credits for your orders; d) you can return products you have problems with, even if opened; and e) I have contacted many supplement manufacturers to ask about recommended online retailers (because I’ve read some scary articles about knock-off supplements on Amazon) and almost all of them have told me Pure Formulas is reputable. Last thought: if you comment below with your Pure Formulas referral code I will use one whenever I order (which is often).
Best Endocrinologist Ever.
Every time I have an appointment with my endocrinologist, I hem and haw about whether I should cancel it. It’s on the other side of town, $50 round-trip in an Uber, it only ever lasts about 20 minutes and couldn’t she just look at my thyroid lab results and email me about whether to stick with my current hormone dosages? Well, each time I go, I am so grateful for this doctor (last week I told her nurse I would walk on hot coals for Dr. B) and I vow to come straight home and write an update so I can remember everything she said. I never have managed to do this and the visit summaries hardly mention anything at all, so today I’m going to write a general update of her treatment.
I’ve seen a lot of endocrinologists in the last six years and they have all, without exception, been kind of odd, stoic and monosyllabic. Until Dr. B. She’s vibrant and engaged (after seeing her, I always mourn my lack of brain energy a little more), listens closely, talks about her ideas out loud, thinks outside of the box and is interested in conditions not typically related to the endocrine system. Imagine that: a big hospital allopathic endocrinologist taking the whole body into account!
The first time I saw her a year ago, I told her my basic story (anaphylaxis 2001-2002, vasovagal collapse 2005-2011, thyroid goiters 2009, radioiodine ablation 2010, SICK 2011), assuming she’d check my thyroid and update my prescription as per usual — and she did, but she also ordered pituitary blood tests, a Cortrosyn stimulation test (CST) (otherwise known as an ACTH stimulation test — it measures how well the adrenal glands respond to ACTH), referred me to two neurologists — one that specialises in headaches and one that specialises in dysautonomia — and said we would consider placing a continuous glucose monitoring device to assess the drops in my blood sugar (good news is, my blood sugar crashes got much better, possibly because I am eating all foods again and have put on weight). No other endocrinologist had ever suggested any of these things.
I was dreading the CST because of my reactivity and intravenous injections of anything don’t allow me to start low and slow, but it was fine. I did my research beforehand (yes, they were they only using 1mcg of Cortrosyn; no, I didn’t need to fast; no, it didn’t need to be timed according to the follicular phase of my menstrual cycle; no, I didn’t need to be off bioidentical hormones; and, yes, my husband could be with me), so I felt comfortable about the procedure and the results were normal.
The pituitary testing showed low LH (luteinizing hormone), DHEA and IGF-1. Because of the latter, at our next appointment Dr. B ordered a pituitary MRI to “leave no stone unturned” (LOVE her). The MRI was normal, but she emphasised that it was less reliable because of my unwillingness to use contrast (I didn’t think the risks of a reaction outweighed the benefits of a better MRI — and she was ok with that). She also gave me a prescription for Florinef to see if it would help with my hypotension (blood pressure was 80/60 at this appointment). I trialed it for a month (starting at 0.0125mg (!!), working up to 0.1mg) and thought it might be increasing my headaches (but not my blood pressure, of course), so I stopped, but it’s still on my list to retry.
My thyroid levels have consistently been tanked for the last 6 years and at every appointment Dr. B would tweak my meds. I’ve gone from 50mcg/day of levothyroxine to 100 to 125 and from 5mcg/liothyronine to 10 and — this is exciting — when I told her my naturopath suggested much higher T3 and lower T4, Dr. B said, “I’m totally open to that, let’s try it.” 😮 Typically allopathic endocrinologists and NDs do not see eye to eye on treatment and optimal thyroid levels and often one doctor will be resistant to another doctor’s suggestions, especially when the suggestion comes from someone who isn’t a specialist. Dr. B has no ego getting in the way. So, we increased my T3 to 15mcg twice/day and lowered T4 to 100mcg. I really don’t know if it has helped, but she seems more satisfied with my thyroid levels. She told me to watch out for tremors, heart palpitations and insomnia, but they are all within my normal constellation of symptoms, so who knows (although, as I’m typing this, I realise that my quite-vicious nightly palpitations haven’t happened in a while– maybe weeks). She diagnosed me with “euthyroid sick syndrome” which essentially means your thyroid will stay sick until the underlying chronic illness gets better.
I saw a headache neurologist and a dysautonomia specialist (more on both of those in separate posts), but neither of them were the ones to which Dr. B referred me. And — another reason to love her — she had no problem with that and was still interested in what they had to say. Even better, when I told her the dysautonomia specialist didn’t have much to offer and essentially told me just to make sure I don’t decondition any further, Dr. B raised her eyebrows in surprise and kind of dismissed this, still interested in helping me fix this piece of the puzzle (those of you that haven’t done the doctor rounds might not realise that almost all of them tell you to simply exercise more (or gain/lose weight) (or take antidepressants), so I expected Dr. B to take the specialist’s assessment as bible and agree that I was just deconditioned). She suggested I do a growth hormone challenge (it involves a 17-hour fast, an 8am check-in and a 5-hour test where they give intravenous glucagon and then measure human growth hormone (HGH) response through blood draws) and said the worst side effect she’d seen was vomiting. I wanted to vomit at the thought of getting to a hospital at 8 in the morning. I went home to do some research; that was in July of last year.
When I saw her again at the end of September, I hadn’t done the HGH challenge and she didn’t give me a hard time at all. Three months after that appointment I still hadn’t found the nerve, so I emailed her a long message about my glucagon fears (those of you with mast cell/anaphylaxis/medication sensitivity issues can read my email* below for the reasons it gave me pause) which any other specialist would either not answer or reply that I should come in for an appointment to discuss. Instead, she sent me a very thoughtful, validating reply (not “For fuck sake, stop being such a scaredy-cat and do the bloody test since I’m the one doctor who is investigating all these things!”) and offered an alternative to glucagon — an insulin challenge test — which I agreed to … and then never did. They give you intravenous insulin, drop your blood sugar to 40 and then test HGH. I told her I was more comfortable with the devil I knew (hypoglycemia) then the one I didn’t. But, it turns out I’m not really comfortable with voluntarily meeting any devil. I’ve had my blood sugar drop into the 40s. It was absolutely horrific — one of the worst feelings I’ve ever felt. And, although they give you intravenous glucose right afterwards, I still couldn’t bring myself to do this test and subject myself to the crash when I thought they probably wouldn’t find anything.
So, I waited until my appointment this month — 8 months after she first wanted to investigate this avenue — and told her of my fears about the insulin challenge test as well. I expected her to just give up, to say there’s probably nothing wrong there, anyway, but she didn’t. She said there was an additional reason to do the insulin challenge (other than for HGH output) and that was that it can pick up a hypothalamus issue that the glucagon stimulation test can’t. Ok, I can get on board since it’s a two-fer. However, in another display of out-of-the-box-ness and medical generosity, she suggested I just try HGH injections without doing the challenge test. She said she had two other patients with the dyautonomia-mast cell-EDS trifecta (more on my EDS diagnosis at another time) and, even though neither one flunked the stimulation test, they tried HGH and had really good results. A friend of my sister-in-law’s had a lot of success with HGH and it has always been in the back of my head as something to try when I win the lotto. I read it cost thousands of dollars, but Dr. B’s prescription is “only” $138/month, so I’m on board. If/when I get the nerve, I can stop the HGH for a week and do the challenge test and, if I fail, insurance will pay for my prescription. An added bonus is my nurse who comes to my home every week (to give me intravenous fluids with my immunoglobulin infusions) can show me how to subcutaneously inject the HGH and I don’t need to go across town for a tutorial appointment.
Gratitude for good doctors! Wish me luck with the HGH.





