A note about my eye exam today:
I need to update my blog more often — for myself, more than anyone else. This morning, I had my first eye exam in 7 years and I looked back here to see if I’d said anything about the last time and saw I’d had a reaction to the yellow eye drops. I had no memory of this and it saved me from possibly having another reaction today for a not-really-needed test. So, I’m going to make a note about today’s experience to remind myself in the future not to bother going to an ophthalmologist again!
My vision was 20/15 the last time I had my eyes checked. I never needed glasses at all until July of 2020, when I realised I couldn’t see my vein very well when putting in a peripheral IV catheter to do IVIG. Since then–not even 2 years–I’ve gone up 3 magnification strengths and my right eye has significantly worse vision than the left. My distance vision is a little worse, too, which I realised when my husband (who is 12 years older than I am) could make out signs on the highway that I couldn’t.
Of course, this is totally normal for people my age, but my brother started to need glasses after spending time on a submarine and had a theory that it was because he didn’t focus on anything more than about 8 feet away for so many months. I think this might hold some truth for those of us who spend so little time outside, looking at horizons and focusing on long distances.
I have a ton of eye symptoms, which bother me much more than the need for readers, but I’ve been told there is no remedy for any of it (except dry eyes). I was told in the past: “When your overall health is poor, your eye health is poor, too.” The ophthalmologist today actually said that my eye health was good, but my symptoms are probably neurological (migraines, dysautonomia etc).
Some of my eye symptoms are: floaters; blurriness; pain in orbital muscles when moving my eyes; itchy eyelashes; dry eye to the point that when I blink in the mornings, my tears feel like acid hitting my eyeballs; right eyelid spasms; light sensitivity; trouble tracking when scrolling on my phone or reading blocks of text; migraines that feel like my right eye is going to explode out of its socket (it’s silly, but I often push my eye back in with the palm of my hand because it really feels like it might pop out). I used to say that my eyes felt like I’d put grit into Vaseline and then smeared it over my eyes.
I have had radioiodine ablation on my thyroid for Graves disease (or some sort of autoimmune presentation of hyperthyroidism–endocrinologists have disagreed on whether it’s actually Graves) and was told to pay attention to eye symptoms, but the doctor today didn’t see any evidence of that being a problem. I am also positive for one of the Sjogren’s markers (carbonic anhydrase VI IgG antibodies), which ophthalmologists treat no differently than dry eye. He rattled off a bunch of things that I’ve tried in the past that have done nothing (eye drops, eye scrubs) and some I haven’t (take omega 3s, humidifier in bedroom).
He said my optic nerves, blood vessels, maculae etc were all normal. During the visual acuity test, none of the letters were sharp, but I could guess most, even though they were blurry. The doctor said my vision was considered 20/20 because I could guess 3 out of 5 of the bottom line, adding he wouldn’t be able to see any of them at all. This is the thing when you’ve had great vision your whole life–you don’t really know what is “normal” or acceptable.” I hate not being able to see the letters clearly, but being able to guess them at all, even though I was straining and it was very blurry, is still considered 20/20.
They said I am doing no damage to my eyes using the cheapo 3-pack of Costco reading glasses. It doesn’t matter what strength I use or whether I use different magnifications (I have various glasses scattered in different rooms) or whether I’m using the lenses that work for one eye, but not the other. Essentially, if you can move the phone/book closer or further away and make it work, then everything’s fine. They said I could get prescription glasses, but, if I’m getting by, there is no need. I don’t want any more energy expenditure on anything, so I’m sticking with what I’m doing. My husband was mildly alarmed by this: But if you can get prescription glasses that correct for the differences in your eyes and it makes your life better, why not? Energy is why not. It all comes down to having nothing extra to give.
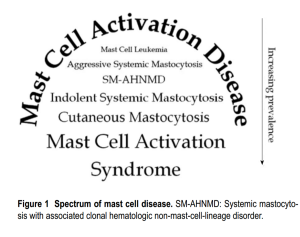
For anyone with MCAS, I have had the yellow eye drops 3 times and, the last time, I had a reaction. A friend told me I could ask for a retinal scan in lieu of dilation, which I did and it was easy and only took a few minutes. Once in the past, I was told that one of my eyes had high pressure (intraocular fluid pressure) and this can be a warning for glaucoma and I should keep an eye on it (I just caught that totally unintended pun when I did a reread 🙂 ). The gold standard for checking eye pressure is the use of yellow numbing eye drops, which are used with a slit lamp and blue light. A step down from that is a handheld tonometer, which still needs numbing drops, but they don’t have the yellow dye. Lastly, there is a device called an Icare, which doesn’t need drops at all. The latter would have been my preference since I don’t know what caused the previous reaction (the dye, the numbing medication or the preservatives), but they didn’t have one at the location where I had my appointment today, so I decided to skip the pressure check, thinking/hoping I probably don’t have a problem.
Lastly, I want to note that this was BY FAR the most risky covid exposure I’ve had (or, really, just human germ exposure, in general). The rooms are tiny with no windows or ventilation and the doctor and his assistant both had to get very close to my face. Also, they cancelled my appointment last week because the ophthalmologist was out sick and I wonder — out sick with what? Even a head cold would be a deal-breaker for me. All in all, I regret the appointment because the risk of contracting a virus was very much outweighed by the chances that I have eye problems that can be remedied (I now know). But I didn’t know what was normal or should be treated and I certainly would want to know if intracranial hyper/hypotension was causing any eye damage (as seen on a CINE MRI, I have blocked cerebral spinal fluid flow in my brain because of low-lying cerebellar tonsils, which can cause intracranial pressure issues). I didn’t know if wearing shitty readers could damage my eyesight further (they can’t) and I didn’t know if having worse vision in one eye was a concern (it’s not) and I didn’t know if I could brush off all of my eye symptoms as neurological (I can). Now I know and you do, too. 🙂 Title Credit