Here are the tests I had done in the first year and a half of my illness.
They were all negative or normal unless otherwise stated:
MALARIA SCREEN (3 times, because the first test was positive. Second two tests were negative)
COMPREHENSIVE METABOLIC PANEL
CBC, DIFF (three times)
SED RATE
G6PD SCREEN
CRP, HIGH SENSITIVITY (multiple times)
COMPLETE URINALYSIS
PROTEIN ELECTROPHORESIS
CULTURE:BACT – BLOOD
RHEUMATOID FACTOR (twice)
ANA REFLEX COMP
ANA PATTERN BY IF (is that the same thing as above?)
ABS TO NUCLEAR AGS
THYROID STIMULATING HORMONE
T3
T4
PARATHYROID HORMONE
CORTISOL
EPINEPHRINE
NOREPINEPHRINE
DOPAMINE
METANEPHRINE
NORMETANEPHRINE
5-HIAA
VITAMIN D
CHEST X-RAY
QUANTIFERON TB TEST
CT SCAN OF CHEST, ABDOMEN AND PELVIS W/ CONTRAST
ULTRASOUND ABDOMEN BACK WALL (looking at benign cyst on kidney)
ZINC (low)
VITAMIN B12
FERRITIN (low)
HEPATITIS C
HEPATITIS B
HIV (TWICE)
ANTI tTRANSGLUTAMINASE, IgA
TTG AB IgA (is that the same thing as above?)
ALLERGEN PANEL (BLOOD TETS): IgA (showed allergies to eggs, cod fish and tomatoes)
ALLERGEN PANEL: SKIN PRICK TESTS (showed allergies to dogs, cats, dust mites, molds, grasses, trees (specifically, alder, birch and red oak))
BLOOD EXAMINED FOR THE FOLLOWING PARASITES: MALARIA, BABESIA, TRYPANOSOMES, MICROFILARIA, BORRELIA
FOLLICLE STIMULATING HORMONE LEVEL
LYME DISEASE (TWICE)
EHRLICHIA
CYTOLOMEGA VIRUS (CMV)
SYPHILIS
EPSTEIN-BARR VIRUS (EBV) (positive for past infection)
IBD SEROLOGY
CPK CARDIAC MARKERS
LIPID PANEL
LIVER PANEL
ELECTROLYTES
HLA B27
ESTIMATED GFR
C-REACTIVE PROTEIN
URIC ACID
CREATININE
STOOL SAMPLE: PANCREATIC ELASTASE 1, PUTREFACTIVE SCFAS, EOISINPHIL PROTEIN X, CALPROTECTIN, BENEFICIAL SCFAS, N-BUTYRATE, PH, BETA-GLUCURONIDASE, LITHOCHOLIC ACID (LCA), DEOXYCHOLIC ACID (DCA), LCA/DCA RATIO, ALPHA HAEMOLYTIC STREPTOCOCCUS, GAMMA HAEMOLYTIC STREPTOCOCCUS, E.COLI, SACCHAROMYCES CEREVISIAE (more than doc would like), BIFIDOBACTERIUM (doc says I don’t have enough), LACTOBACILLUS SPECIES (no growth ~ doc says this is dangerous)
————————————————————————————————————————————————————————————————————————————————————————————————————————————
March, 2013 tests:
1) Cortisol too high at night ~ take phosphorylated serine (a supplement called Seriphos made by Interplexus, 1/2 a pill (apx 500mg) about an hour before I go to sleep (led to a harder time getting to sleep as well as more frequent wakings, as well as fewer overall hours sleep) or phosphatidylserine 100 mg 30-60 minutes before bedtime).
2) Gut dysbiosis ~ continue doing what I’m doing, possibly cutting out soy.
3) 17-hydroxyprogesterone was 22 with a range of 22-100, but doctor didn’t think it meant anything.
Other results:
IgA antibody for milk, eggs, gluten =negative. Soy = equivocal.
DHEA was 6 range of 3-10.
17-hydroxyprogesterone was 22 with a range of 22-100.
H. pylori was low = negative.
When my stool was cultured for yeast, it was negative.
Estrodial was 8 range or 2-10.
Progesterone was 45 range of 20-100.
Chymotrypsin was 12 range being >9.
No signs of parasites or infectious disease-causing bacteria.
Levels of two enzymes (lysozyme and alpha-lactalbumin, I think?) that the gut produces when it’s irritated were low = good.
My bacterial balance indicates gut dysbiosis. Low in friendly gram-positive bacteria and too high in gram-negative bacteria.
Salivary cortisol test:
Morning = 16 Range 13-24
Noon = 10 Range 5-10
4pm = 8 Range 3-8
12am = 7 Range 1-4
3/14/2013: Vitamin D 30.6 ng/mL; Vitamin D 1,25 42 pg/mL (range 17-72) (Functional medicine says 50-75)
4/9/2013: Iron 99 (range 35-155) Ferritin 64 (range 13-150); vitamin B12 1364 (range 211 – 946 pg/mL); zinc 1165 (822 – 1571 ug/dL)
9/26/2013: Vitamin D 30.3 (range 30.0 – 100.0 ng/mL)
7/10/2013:
- Copper 94 mcg/dL (range 80-155)
- Transthyretin (Pre Albumin) 26 mg/dL (range 18-39)
- Magnesium 2.3 mg/dL (range 1.8-2.4)
- BMP:
- Sodium, Plasma 142 (136 – 145 mEq/L)
- Potassium 3.8 (3.7 – 5.2 mEq/L)
- Chloride 107 (98 – 108 mEq/L)
- Carbon Dioxide 28 (22 – 32 mEq/L)
- Ion Gap 7 (3 – 11)
- Urea Nitrogen 7 (8 – 21 mg/dL)
- Creatinine 0.62 (0.38 – 1.02 mg/dL)
- Calcium 9.5 (8.9 – 10.2 mg/dL)
11/5/2013: Methylation pathway blood test ~ Health Diagnostics and Research Institute:
- Glutathione (oxidised) 0.30 (0.16-0.50)
- Glutathione (reduced) 3.2 (3.8-5.5)
- S-Adenosylmethionine 219 (221-256)
- S-Adenosylhomocysteine 37.7 (38-49)
- Folic Acid derivitives:
- 5-CH3-THF 10.7 (8.4-72.6)(Doctor thought this was low)
- 10-Formyl-THF 1.8 (1.5-8.2) (Doctor thought this was low)
- 5-Formyl-THF 1.0 (1.2-11.7)
- THF 0.63 (0.6-6.8)
- Folic Acid 9.7 (8.9-24.6)
- Folinic Acid 7.0 (9-35.5)
- Active folate 358 (400-1500)
- Adenosine: 20.8 (16.8-21.4)
11/6/2013: Adrenal saliva test ~ Diagnostechs
Cortisol elevated at night and slightly in afternoon after carbohydrate challenge. That would explain trouble sleeping at night but in the afternoon doesn’t quite make sense. Phosphatidylserine 100 mg to start 15 to 20 minutes before meals within 1 to 2 hours of elevated cortisol time which are 11-1 pm and the 10pm to midnight range.
11/08/2013: Abdominal ultrasound for upper right quadrant pain. Everything normal. Benign angiomyolipoma on left kidney.
11/13/2013: Mycotoxin urine test ~ Realtime labs:
- Ochratoxin 5.25 (1.8-2.0) Positive
- Aflatoxin 0.98 (0.8-1.0) Equivocal
- Tricothecene 0.53 (0.18-0.2) Positive
11/18/2013-ish: 23andme saliva test
11/27/2013: Allergy testing from Medscape:
- For angioedema without urticaria (especially those with recurrent episodes), diagnostic tests should include the following:
- C4 level: they forgot to do this one.
- C1 esterase inhibitor (C1-INH) quantitative and functional measurements: “C1 inhibitor, functional >100%” (normal); “C1 esterase inhibitor, protein 23 mg/dL” (range 21-39)
- C1q level: 7.9 mg/dL (range 5.0-8.6) Normal
From what I can tell, these results mean that I do NOT have hereditary angioedema (although, it does not exclude type III) and I do not have acquired angioedema, so it is idiopathic and was confirmed autoimmune with plasma injected under my skin, which caused an allergic reaction.
- Tryptase enzyme immunoassay, alpha and beta forms: 4 ng/mL (range 2-10)
- Cauliflower, broccoli, coconut, egg white, cod, oat, tomato IgE: all <0.35 kU/L Normal (note: egg, tomato and cod were all positive 2 years ago and I haven’t eaten them in 1.5 years).
1/08/2014:
- TSH 0.977 (0.34-5.6)
- Free T3 3.7 (2.2-4.3) low: want it 3.7-4.2
- Free T4 0.56 (0.57 – 1.25) low: want it 1.3-2.8
1/27/2014:
- Baseline 24-hour urine tests for (NOT during an episode):
- n-methylhistamine: 146 mcg/g Cr (30-200)
- prostaglandin D2 (PG D2): 153 ng/24 h (100-280)
- BPG2 concentration: 148 pg/mL
- 11 beta-prostagladin F2 Alpha: 350 ng/24 h (< or = 1000)
- NTX: 92
- NTX-telopeptide: 26 (19-63)
- urine calcium: 125 (42-353)
- Creatinine: 40 mg/dL
- Creatinine conc: 41 mg/dL
- Serum:
- General
- Magnesium 2.1 mg/dL (1.9-2.5)
- PTH 33 pg/mL (14-72)
- Calcium 9.1 mg/dL (8.3-10.2)
- CRP < 0.3 mg/dL (0.0-1.2)
- IgG 676 mg/dL (600-1700)
- IgA 114 mg/dL (87-474)
- IgM 190 mg/dL (40-250)
- ACE (angiotensin Cnv Enz) 47 U/L (8-53)
- S Cerevisiae IgA <10 (<=20.0 = neg)
- S Cerevisiae IgG 33.6 (<=20.0 = neg)
- Nuclear Antigen Panels
- Abs to Nuclear Ags: neg
- ANA by IF and mulitplex: none/neg
- Celiac Testing
- TTG Ab IgA <1.2 U/mL (<4.0=neg)
- TTG Ab IgG <1.2 U/mL (<6.0=neg)
- Endomysial Ab: neg
- ANCA panel for vasculitits
- c-ANCA neg
- p-ANCA neg
- General
- Spine xray (nothing significant)
- Dexa bone scan (osteopenia):
- Neck of hip T score: -2.0 (was -2.3 in 2010!)
- Hip T score total: -1.4 (was -1.1 in 2010)
- Spine T score total: -0.4 (was -0.1 in 2010)
- Ultrasound of shoulders (bursitis ~ doctor suggested cortisone injections or prednisone)
5/23/14 Dr. Erin: Histamine, blood: 50 ng/mL (12-127) Dr. Erin says to ignore the range, that 50 is borderline high.
6/1/14: 24-hour urine collection, Dr. Erin:
- Lead: None detected
- Creatinine: 0.32 g/L (0.30-3.00) Low creatinine is seen in conditions with decreased muscle mass.
6/3/14:
- Beta-hydroxybutyrate 0.40 (0.00 – 0.20 mmol/L)
- Insulin 2.1 (0.0 – 24.9 uIU/mL)
- Taurine 103 (30 – 110 mcmol/L) Yasko says aim for <50%
- Vitamin B2 1.00 (1.00-1.30)
- Vitamin D3 (25_Hydroxy) 49.1 (20.1 – 50.0 ng/mL) I have read NDs want it around 80
- Iron Panel:
- Ferritin 44 (10 – 180 ng/mL) NDs say aim for >/=50
- Transferrin 243 (192 – 382 mg/dL)
- Iron SRM 90 (40 – 155 mcg/dL)
- Total iron binding capacity 340 (270 – 535 mcg/dL)
- Transferrin saturation 26 (10 – 45 %)
- Lipid panel:
- Cholesterol (Total) 257 (<200 mg/dL)
- Triglyceride 38 (<150 mg/dL)
- Cholesterol (HDL) 88 (>40 mg/dL)
- Cholesterol (LDL) 161 (<130 mg/dL)
- Non-HDL Cholesterol 169 (0 – 159 mg/dL)
- Cholesterol/ HDL Ratio 2.9
- Thyroid Panel:
- T4, free 0.6 (0.6 – 1.2 ng/dL) low: want it 1.3-2.8
- T3, free 3.1 (2.3 – 3.9 pg/mL) low: want it 3.7-4.2
- TSH 0.590 (0.400 – 5.000 uIU/mL) Trying to be 1.0
- Anti Thyroid Peroxidase 1.7 (0.0 – 8.9 IU/mL)
- Anti thyroglobulin <1.0 (0.0 – 3.9 IU/mL)
- BMP:
- Sodium, Plasma 140 (136 – 145 mEq/L)
- Potassium 3.2 (3.7 – 5.2 mEq/L)
- Chloride 105 (98 – 108 mEq/L)
- Carbon Dioxide 27 (22 – 32 mEq/L)
- Ion Gap 8 (3 – 11)
- Glucose 83 (62 – 125 mg/dL)
- Urea Nitrogen 4 (8 – 21 mg/dL)
- Creatinine 0.59 (0.38 – 1.02 mg/dL)
- Calcium 9.4 (8.9 – 10.2 mg/dL)
6/15/14: 24-hour urine collection. Dr. Erin:
- Porphyrins: Hexacarb (6-CP) was high at <4, but she said not to worry about it.
- Delta ALA: 1.8 mg/24 hr (0.5-5.1)
- Porphobilinogen (PBG):
- Quantitative: 0.1 mg/L (0.0-2.0)
- 24U: 0.3 mg/24 hr (0.0-1.5)
7/7/14: Dr. Chia
- Chlamydia pneumoniae IgG and IgM Negative
- Coxsackie B-1 Ab <1:10 Negative
Coxsackie B-2 Ab <1:10 Negative
Coxsackie B-3 Ab Negative
Coxsackie B-4 Ab >=1:640 Very High
Coxsackie B-5 Ab 1:160 High
Coxsackie B-6 Ab <1:10 Negative - Echovirus, Serum Ab (6, 7, 9, 11, 30) Negative
- Creatine Kinase, total 27 (24-173)
- CRP, quant <0.8 (0.0-4.9)
- HHV6 IgG antibodies 8.27 (<0.76) Very High
- IgG total: 747 (700-1600) Dr. Chia says all of these are low.
- IgG subclass 1: 409 (422-1292)
- IgG subclass 2: 221 (117-747)
- IgG subclass 3: 14 (41-129)
- IgG subclass 4: 7 (1-291)
- Immunoglobulin A, Qn 114 (91-414)
- CMV IgG and IgM Negative
- T-lymph Help/Supp-short
- Absolute CD3 1365 (622-2402)
- Absolute CD4 566 (359-1519)
- Abs CD 8 supressor 687 (109-897)
- % CD 3 Pos. Lymph 80.3 (57.5-86.2)
- % CD 4 Pos. Lymph 33.3 (30.8-58.5)
- % CD 8 Pos. Lymph 40.4 (12-35.5)
- CD4/CD8 Ratio 0.82 (0.92-3.72)
- Lymphs Absolute 1.7 (0.7-3.1)
7/10/14: Dr. Erin
Varicella Zoster IgG 1488 (positive >165)
Varicella Zoster Ab, IgM 1.68 (positive >1.09)
HSV, IgM I/II combo 1.38 (positive >1.09)
HSV 1 IgG Negative
HSV 2 IgG Negative
Coxsackie A7 IgG 1:800 High
Coxsackie A9 IgG 1:800 High
Coxsackie A16 IgG 1:800 High
Coxsackie A24 IgG 1:1600 High
Coxsackie B-1 Ab 1:16 High
Coxsackie B-2 Ab 1:8 High
Coxsackie B-3 Ab Negative
Coxsackie B-4 Ab Negative
Coxsackie B-5 Ab 1:32 High
Coxsackie B-6 Ab 1:32 High
EBV Ab VCA, IgM Negative
EBV Early Antigen Ab, IgG 68.7 (0.0-8.9)
EBV Ab VCA, IgG 396 (0.0-17.9)
EBV Nuclear Antigen Ab, IgG 172 (positive >21.9)
Interpretation = Convalescence/Pas Infection or Reactivated Infection
HHV 6 IgG Ab 7.49 (positive >0.99)
HHV 6 IgM Negative
Cytomegalovirus (CMV) Ab, IgG Negative
CMV Ab, IgM Negative
Parvovirus B19, IgG 0.3 Negative
Parvovirus B19, IgM 0.2 Negative
Chlamydia pneumonae IgG Negative
Chlamydia pneumonae IgM Negative
Chlamydia pneumonae IgA Negative
HNK1 (CD57) Panel
%CD8-/CD57+ Lymphs 5.0 (2.0-17.0)
Abs. CD8-CD57+ Lymphs 75 (60-360)
Antistreptolysin O Ab 113.2 (0.0-200)
Neutrophils 75 (40-74)
CBC, Platelet Count and Diff all normal except neutrophils:
(WBC,RBC,Hemoglobin,Hematocrit,MCV,MCH,MCHC,RDW,Platelets,Neutrophils,Lymphs,Monocytes,Eos,Basos,Neutrophils Absolute,Lymphs Absolute,Monocytes Absolute,Eos Absolute,Baso Absolute,Immature Granulocytes,Immature Granulocytes Absolute)
7/31/2014: Hormone test, Dr. Erin (Day 7 of 32-day cycle):
- Pregnanediol 0.27 (0.70-7.10)
- DHEA
- (0.20-1.60)
- Androsterone 2.18 (2.30-9.70)
- Eitocholanolone 1.50 (2.40-9.40)
- 11-Etiocholanolone 1.50 (2.40-9.40)
- 11-keto-etiocholanolone 0.38 (0.30-1.80)
- 11-hydroxy-androsterone 0.86 (1.30-4.80)
- 11-hydroxy-etiocholanolone 0.48 (0.50-2.70)
- 17-Ketosteroids 5.5 (9.9-30.6)
- Testosterone 0.09 (0.16-0.65)
- Androstanediol
- Pregnanetriol 0.42 (1.00-3.90)
- allo-Tetrahydrocortisol a-THF 0.98 (1.10-5.60)
- Tetrahydrodeoxycortisol THS 0.18 (<=1.20)
- Tetrahydrocortisol THF 1.51 (2.40-7.00)
- 17-Hydroxysteroids, total 13.1 (10.2-23.6)
- Cortisol, Free 24 (20-90)
- Estrone 10.0 (2.0-39.0)
- Estradiol 2.2 (1.0-13.0)
- Estriol 3.9 (3.0-48.0)
- 2-Hydroxyestrone 25.8 (9.2-76.6)
- 16alpha-Hydroxyestrone 25.0 (2.4-20.3)
- 4-Hydroxyestrone 9.3 (<=5.3)
- 2-Methoxyestrone 1.2 (>=1.7)
- 4-Methoxyestrone
- =1.9)
- Anabolic/Catabolic Balance 0.4 (1.0-3.9)
- 11beta-HSD Index 0.25 (0.93-1.37)
- E/A: 5beta/5alpha Ratio 0.7 (0.7-1.9)
- 2-Hydroxyestrone/16alpha-hydroxyestrone Ratio 1.0 (1.7-2.8)
- 2-Methoxyestrone/2-Hydroxyestrone Ratio 0.05 (>=0.09)
- Aldosterone 3.6 (6.0-44.0)
- Triiodothyronine, T3 1,742 (732-4,750)
8/13/2014 Dr. Lisa
Ammonia 17 (5 umol/L)
Potassium 4.2 (3.1 – 5.1 mmol/L)
Homocysteine 6.1 (3.5 – 11.0 umol/L)
10/2/14: Dr. Erin (day 12 of 47-day cycle; spotting days 11-13, possible ovulation?):
CBC, Platelet Count and Diff all normal
Iron Binding Capacity (TIBC) 258 (250-450)
UIBC 186 (150-375
Iron, Serum 72 (35-155): Was 99 in 2013 and 90 in June, 2014.
Iron, Saturation 28 (15-55)
Ferritin, Serum 60 (15-150)
TSH 0.358 (0.450-4.5)
Free T3 1.8 (2.0-4.4) low: want it 3.7-4.2
Reverse T3 11.1 (9.2-24.1)
Free T4 0.71 (0.82-1.77) low: want it 1.3-2.8
DHEA 254 (31-701)
DHEA-sulfate 50.6 (57.3-279.2)
Progesterone 0.2 Day 12 (after spotting, with next period very late) (follicular phase 0.2-1.5) (ovulation phase 0.8-3.0)
Estradiol 73.3 (follicular phase 12.5-166) (ovulation phase 85.8-498)
Estrogens, total 172 (122-437)
Estrone, Serum 39 (follicular phase 37-138) (Mid-cycle 60-229)
Testosterone, Serum 4 (8-48)
Free Testosterone Cortisol 16.9 (6.2-19.4)
IgG Qn, Serum 709 (700-1600) lower than when Dr. Chia took it.
11/11/14: Dr. Kim
CBC with Diff: All normal
Metabolic Panel: All normal(potassium 4.2) except:
Albumin/Globulin ratio: 2.7 (1.1-2.5)
Alkaline Phosphatase: 34 (39-117)
Candida Antigen: Negative
Candida Ab IgG: <30 (0-29)
Candida Ab IgM: 10 (0-9) High
Candida Ab IgA: 23 (0-9) High
Dr. Kim is putting me on Nystatin.
IgG subclass 1: 378 (422-1292): lower than July, 2014.
IgG subclass 2: 203 (117-747): lower than July, 2014.
IgG subclass 3: 14 (41-129): exact same as July, 2014.
IgG subclass 4: 7 (1-291): exact same as July, 2014.
IgG total: 697 (700-1600): lower than last 2 times it was checked.
EBV Ab VCA, IgM: <36.0: Negative
EBV Early Antigen Ab, IgG: 52.2 (0.0-8.9) High
EBV Ab VCA, IgG: 414.0 (<18.0) High
EBV Nuclear Antigen Ab, IgG: 119.0 (<18.0) High
Interpretation = “Reactivated Infection” Dr. Kim says I’m “dripping in EBV.”
IgA: 95 (91-414)
IgM: 197 (40-230)
IgE: 17 (0-100)
Mycoplasma Pneumoniae IgG Abs: 355 (0-99) High
Mycoplasma Pneumoniae IgM Abs: Negative
Cytomegalovirus (CMV) Ab IgG: Negative
Cytomegalovirus (CMV) Ab IgM: Negative
Human Herpes Virus Type 6 (HHV6) IgM: Negative
HHV6 IgG Ab: 12.14 (<0.76) Very high
Antistreptolysin O Ab 109.6 (0.0-200.0)
Lyme, Western Blot: negative (again)
Babesia microti IgM: Negative
Babesia microti IgG: Negative
Reverse T3: 11.1 (9.2-24.1)
LDH: 119 (119-226)
Hemoglobin A1c: 5.3 (4.8-5.6)
Magnesium, RBC: 6.3 (4.2-6.8)
Zinc, RBC: 1199 (822-1571)
Vitamin D, 25-Hydroxy: 43.5 (30-100): Was 30.6 and 30.3 in 2013, 49.1 in 6/2014.
Folate, RBC: 832 (499-1504)
Folate, Hemolysate: 297.7
Iron Binding Cap: (TIBC): 308 (250-450): Was 340 in 6/2014 and 258 in 10/2014.
UIBC: 240 (150-375): Was 186 in 10/2014.
Iron: 68 (35-155): Was 99 in 2013, 90 in 6/2014, 72 in 10/2014.
Iron Sat: 22 (15-55): Was 26 in 6/2014 and 28 in 10/2014.
Ferritin: 48 (15-150): Was 64 in 2013, 44 in 6/2014, 60 in 10/2014.
12/1/14: Dr. Erin:
TSH 0.063 (0.450-4.5)
Free T3 2.2 (2.0-4.4) low: want it 3.7-4.2
Free T4 0.94 (0.82-1.77) low: want it 1.3-2.8
1/26/15 Dr. Erin (day 33 of 38-day cycle: luteal phase):
Lipid Panel:
Total LDL 194 (<130)
LDL4+3+2+1 175 (<100)
IDL 11 (40)
HDL2 41 (>15)
HDL3 62 (>25)
Total VLDL 14 (<30)
VLDL1+2 5.6 (<20)
VLDL3 8 (<10)
Total Cholesterol 310 (<200)
Triglycerides 43 (<150)
Non-HDL Cholesterol 208 (<160)
Remnant lipoproteins 19 (<30)
Lp(a) 9 (<10)
LDL Density (Pattern) A = less risk
Apo B 124 (<109)
Apo AI 219 (>145)
Apo B/AI ratio 0.57 (<0.75)
LDL-P 1755 High (low= <1000)
CBC w/ Diff all normal
CMP:
Glucose 85
Calcium 9.6 (8.5-10.6)
BUN 5.8 (7.0-20.1)
Creatinine 0.7 (0.6-1.1)
BUN/creatinine ratio 8 (12-20)
eGFR 92 (>60)
Sodium 141 (136-145)
Potassium 3.7 (3.5-5.1)
Chloride 105 (98-107)
Carbon dioxide 24 (22-31)
Protein, total 6.8 (6.2-8.3)
Albumin 4.3 (3.4-5.0)
Bilirubin, total 0.6 (0.2-1.2)
AST 15 (5-34)
ALT 14 (0-55)
Alkaline phosphatase 39 (40-150) was 34 on 11/11/14
Testosterone, total 6.46 (5.2-69.2)
Testosterone, free 0.05 (0.04-1.80)
Testosterone, bioavailable 1 (1.2-43.5)
Testosterone, % free 0.8 (0.63-2.65)
SHBG 111 (16-125)
Estradiol 103 (21-312)
Progesterone 3.1 (1.2-15.9)
DHEA-sulfate 62 (75-410)
Cortisol 10.2 (3.7-19.4)
HbA1c 5.1 (<5.6)
Glucose, estimated average 100 (<114)
Insulin 2.5 (3.0-21.1)
LDH 145 (125-220)
Uric Acid 2.8 (2.6-6.0)
Rheumatoid factor <15 (<30)
CRP-hs 0.3 (<1.0)
GGT 9 (9-36)
Ferritin 36 (10-190) Was 64 in 2013, 44 in 6/2014, 60 in 10/2014, 48 in 11/2014.
Homocysteine 10.8 (<10.4) was 6.1 on 8/13/14
Vitamin D, 25 48 (30-96) Was 30.6 and 30.3 in 2013, 49.1 in 6/2014, 43.5 in 11/2014.
TSH 1.71 (0.35-4.94) too high, want to be at 1.00
Free T3 1.81 (1.71-3.71) low: want it 3.7-4.2
Free T4 0.71 (0.70-1.48) low: want it 1.3-2.8
4/13/2015 Endo Dr. B:
ACTH stimulation test: Normal: Cortisol: 9.54 ~> 19.79
Sodium 139 (134-144)
Potassium 3.9 (3.5-5.2)
Chloride 99 (97-108)
Total C02 26 (18-29)
Urea Nitrogen 6 (6-24)
Creatinine 0.64 (0.57-1.00)
Glucose 61 (65–99) this was not fasting and my norm is 80-85
Calcium 9.7 (8.7-10.2)
TSH 1.730 (0.450-4.500) too high, want to be at 1.00
Free T3 1.9 (2.0-4.4) low: want it 3.7-4.2
Free T4 0.81 (0.82-1.77) low: want it 1.3-2.8
Reverse T3 9.8 (9.2-24.1)
(Day 14 and spotting, but of a 38-day cycle)
FSH 6.5 (Follicular 3.5-12.5 Ovulation 4.7-21.5)
Prolactin 5.52 (4.8-23.3) good
LH 5.52 (Follicular 2.4-12.6 Ovulation 14.0-95.6)
DHEA S04 66.2 (57.3-279.2) too low
ACTH 26.8 (7.2-63.3)
IGF-1 109 (41 – 50y Range: 118 – 298 Mean: 205)
eGFR 110.84 (>59) Second test not high
eGFR Black 128.46 (>59)
4/27/2015: Dr. Z: MRI Defecography/pelvis without contrast
Showed anatomical problems and also, possibly, problems with “coordination of muscles.”
1. Tricompartmental pelvic floor dysfunction.
2. Moderate uterine descent.
3. Mild urethral hypermobility. Miniscule cystocele (= bulging of the bladder into the back wall of the vagina).
4. Moderate anterior rectocele (= herniation (bulge) of the front wall of the rectum into the back wall of the vagina).
5. Sigmoidocele is evident (= sigmoid colon pushes down from within the abdominal cavity onto the back wall of the vagina through the gap between the rectum and vagina).
6. Uterus demonstrates multiple cystic lesions in the cervix; possible endocervical glandular hyperplasia.
5/15/2015: Dr. Z: Anorectal Manometry
Mean sphincter resting pressure 95 (45-70mmHg)
Length of HPZ 2.5 (3.4-3.8cm)
Maximum squeeze pressure 148 (120-160mmHg)
Duration of sustained squeeze 14 (>20secs)
First Sensation 60 (30-70mL)
Urge Threshold 160 (80-130mL)
Maximum Tolerated Volume 210 (130-200mL)
Intrarectal pressure 33 (>50mmHg)
Overall Assessment:
No evidence of pelvic floor dyssynergia
Mild rectal hyposensitivity: Consider biofeedback therapy for rectal hyposensitivity.
Decreased squeeze pressures and duration: evaluate for colonic inertia with colon transit study.
6/4/2015: Dr. B
TSH 1.190 (0.450 – 4.500)
Free T3 1.9 (2.0 – 4.4)
Free T4 0.84 (0.82 – 1.77)
IGF-1 133 (62 – 204)
IGF-1 (pediatric esoterix) 134 (118 – 298)
7/14/2015: Dr. B: Brain and pituitary MRI w/o contrast:
Stable nonspecific foci of white matter FLAIR signal hyperintensity involving bilateral frontal lobes signal abnormality, otherwise normal brain MRI.
No pituitary abnormality,however contrast is recommended.
7/14/2015: Dr. J: Cervical spine flexion/extension MRI w/o contrast:
Mild degenerative disc changes resulting in:
Trace degenerative endplate edema at C5-6, right side greater than left.
Small broad-based disc bulge resulting in mild to moderate narrowing of the central canal at C4-5 and mild narrowing at C3-4 and C5-6.
No significant neural foraminal narrowing. No abnormal motion on flexion-extension views to suggest instability. No significant change in central canal narrowing.
7/27/2015: Dr. B:
TSH 1.390 (0.450-4.500)
Free T4 0.94 (0.82-1.77)
Free T3 1.8 (2.0-4.4)
EGFR 113.05 (>59)
EGFR (black) 131.02 (>59)
POTASSIUM 4.4 (3.5-5.2)
TOTAL CO2 24 (18-29)
CREATININE 0.59 (0.57-1.00) Low creatinine is seen in conditions with decreased muscle mass.
CALCIUM 9.4 (8.7-10.2)
UREA NITROGEN 5 (6-24)
SODIUM 140 (134-144)
CHLORIDE 105 (97-108)
8/4/2015: Dr. Erin:
DHEA+DHEA Sulfate 176 (31-701)
DHEA Sulfate 47.1 (57.3-279.2)
Cholesterol, total 219 (100-199) Was 257 in 6/2014, 310 in 1/2015.
Triglycerides 37 (0-149)
HDL cholesterol 93 (>39)
VLDL cholesterol Cal 7 (5-40)
LDL cholesterol Calc 119 (0-99) Was 194 in 1/2015.
Vitamin D, 25-Hydroxy 37.7 (30-100) Was 30.6 and 30.3 in 2013, 49.1 in 6/2014, 43.5 in 11/2014, 48 in 1/2015.
Homocysteine 7.6 (0-15)
Ferritin 29 (15-150) Was 64 in 2013, 44 in 6/2014, 60 in 10/2014, 48 in 11/2014, 36 in 1/2015.
IgG total 685 (700-1600) Was 747 in 7/2014, 697 in 11/2014.
IgA total 105 (91-414)
Magnesium, RBC 6.6 (4.2-6.8)
CBC w/Diff/platelet: all normal ranges.
8/21/2015: Dr. I:
Protein, total 6.1 (6.0-8.5)
Albumin 3.7 (3.2-5.6)
Alpha-1-globulin 0.2 (0.1-0.4)
Alpha-2-globulin 0.6 (0.4-1.2)
Beta-globulin 0.8 (0.6-1.3)
Gamma-globulin 0.8 (0.5-1.6)
M-spike not observed
Globulin, total 2.4 (2.0-4.5)
A/G Ratio 1.5 (0.7-2.0)
IgA 104 (91-414)
IgA, subclass 1 71.9 (73.2-301.2)
IgA, subclass 2 31.9 (13.4-97.9)
9/25/2015: Dr. B:
TSH 0.227 (0.450-4.500)
Free T4 0.83 (0.82-1.77)
Free T3 3.1 (2.0-4.4) (finally!)
EGFR and BMP all normal.
_________STARTED SCIG/IVIG October 1st, 2015____________
11/06/2015: Dr. I:
IgA 124 (66-433)
IgG 849 (635-1741)
IgM 189 (45-281)
11/30/2015: Dr. I:
IgA 124 (66-433)
IgG 968 (635-1741)!!
IgM 187 (45-281)
12/08/2015: Dr. B:
TSH 0.412 (0.450-4.500)
Free T4 0.78 (0.82-1.77)
Free T3 2.1 (2.0-4.4)
1/25/2016: Dr. I:
IgA 120 (66-433)
IgG 1020 (635-1741)!!!
IgM 185 (45-281)
2/26/2016: Dr. B: (a few hours after taking only morning T3, not T4)
IGF-1 (esoterix) 113 (41 – 50 years old: 118-298; mean 205) Low
TSH 0.699 (0.450-4.500)
Free T4 0.57 (0.82-1.77) Low
Free T3 4.7 (2.0-4.4) High
3/7/2016: Dr. I:
IgA 86 (91-414)
IgE 26 (0-100)
IgM 173 (40-230)
IgG 962 (700-1600)
Subclass 1 464 (422-1292)
Subclass 2 274 (117-747)
Subclass 3 16 (41-129)
Subclass 4 13 (1-291)
3/08/2016: Dr. I:
CBC: normal
CMP: all normal except Creatinine 0.56 (0.57-1.00)
Zinc, RBC: 1052 (822-1571)
Magnesium, RBC: 6.4 (4.2-6.8)
Vitamin B12: 377 (211-946)
Ferritin: 30 (15-150) Too low
Iron:
- Iron Bind.Cap.(TIBC) 338 (250-450)
- UIBC 261 (131-425)
- Iron, Serum 77 (27-159)
- Iron Saturation 23% (15-55)
Lipid Panel:
- Total Cholesterol 228 (100-199) High, but better than 310
- Triglycerides 41 (0-149)
- HDL Cholesterol 88 (>39) HDL-C >59 is considered a negative risk factor for CHD.
- VLDL Cholesterol Cal 8 (5-40)
- LDL Cholesterol Calc 132 (0-99) High, but better than 194
Vitamin D:
- 25-Hydroxy 40.4 (30-100) Too low
- 1,25 Calcitriol 48.2 (19.9-79.3)
EBV:
- Ab VCA, IgM <36 (0.0-35.9)
- Early Antigen Ab, IgG 37.9 (0.0-8.9) High
- Ab VCA, IgG 465.0 (0.0-17.9) High
- Nuclear Antigen Ab, IgG 314.0 (0.0-17.9) High
=> Interpretation = Past infection or reactivated infection.
Chlamydia pneumoniae: neg
Mycoplasma pneumoniae:
- IgG 373 (0-99) High
- IgM neg
HHV6:
- IgG 10.13 (positive = >0.99) High
- IgM neg
CMV:
- IgG 2.00 (0.00-0.59) High
- IgM neg
Candida:
- Candida Antigen neg
- IgG <30 (0-29)
- IgM 22 (0-9) High
- IgA 21 (0-9) High
Lyme, Western Blot, LabCorp: Negative (all absent except IgG P41 Ab= present and IgM P41 Ab= present).
Testosterone:
- Total 24 (10-55)
- Free 1.2 (0.0-4.2)
Estrodial: 371.2 (12.5-166) High
Estrogens, Total: 235 (61-394)
Progesterone: 4.6 (0.2-1.5) High
Sex Horm Binding Glob: 124.1 (24.6-122.0) High
Antistreptolysin O Ab: 162.9 (0.0-200.0)
6/13/2016: Dr. Ryan:
24-hour urine tests: Sodium, Potassium, Calcium, Uric Acid, Creatinine all normal.
Creatinine clearance calc. 136 (65-105 mL/min)
Creatinine blood test: 0.60 (0.38-1.02 mg/dL)
6/15/2016: Dr. I, ordered by Dr. B: (about 21 hours after last T3 dose, 25 hours after T4)
TSH 0.743 (0.450-5.10)
T4 1.9 (4.7-11.3) Low
Free T4 0.41 (0.70-1.50) Low
Free T3 2.8 (2.3-4.2)
IGF-1 157.9 (118 – 298 ng/mL)
6/15/2016: Dr. I: (8 days after infusion)
IgA 123 (66-433)
IgG 1110 (635-1741)
IgM 182 (45-281)
IgE 39.6 (0-158)
06/28/2016: Dr. I:
CBC: normal
CMP: normal
Ferritin: 40 (15-150) Too low
EBV:
- Ab VCA, IgM <36 (0.0-35.9)
- Early Antigen Ab, IgG 25.8 (0.0-8.9) High, but down
- Ab VCA, IgG 500.0 (0.0-17.9) Higher
- Nuclear Antigen Ab, IgG 323.0 (0.0-17.9) Higher
Mycoplasma pneumoniae:
- IgG 403 (0-99) Higher
- IgM neg
HHV6: IgG 13.70 Higher
CMV: IgG 2.60 (0.00-0.59) Higher
Candida:
- Candida Antigen neg
- IgG <30 (0-29)
- IgM 17 (0-9) High, but down
- IgA 35 (0-9) Higher
Sex Horm Binding Glob: 162.3 (24.6-122.0) Higher
Antistreptolysin O Ab: 178.6 (0.0-200.0)
8/30/2016: (Dr. R): 24 hour Urine:
Creatinin Interval 24h
Creatinin, Total Volume 3,807 mL
Creatinin/Unit 28 mg/dL
Creatinin/24 Hr 1,066 mg/24h (700-1,800 mg/24h)
10/24/2016: Dr. I:
IgA 125
IgE 38.3
IgM 193
IgG 1169
Subclass 1 764
Subclass 2 346
Subclass 3 13
Subclass 4 33
12/14/2016: Dr. B:
Free T3 2.7 (2.0-4.4 pg/mL)
Free T4 0.78 (0.82-1.77 ng/dL) Low
TSH 0.064 (0.450-4.500 uIU/mL) Low
IGF-1 143 (118-298 ng/mL; Mean: 205)
Lithium none detected (0.6 – 1.4 mmol/L)
12/21/2016: Dr. I:
HHV 6 IgG Antibodies 29.89 High
3/5/2017: Dr. B:
Free T3 2.5 (2.0-4.4 pg/mL)
Free T4 0.82 (0.82-1.77 ng/dL)
TSH 0.033 (0.450-4.500 uIU/mL) Low
IGF-1 130 (118-298 ng/mL; Mean: 205)
Dr. K: 3/30/2017 (8 weeks after last infusion):
Immunoglobulin G 842 (694-1618)
Subclass 1 505 (382-929)
Subclass 2 296 (241-700)
Subclass 3 17 (22-178)
Subclass 4 15.5 (4-86)
CellTrend GmbH
Anti alpha-1-adrenergic AB 11.2 Positive
Anti alpha-2-adrenergic AB 8.9 NEG
Anti beta-1-adrenergic AB 5.6 NEG
Anti beta-2-adrenergic AB 8.0 At Risk
Anti Muscarinic Cholinergic Receptor 1 AB 5.1 NEG
Anti Muscarinic Cholinergic Receptor 2 AB 8.1 NEG
Anti Muscarinic Cholinergic Receptor 3 AB 4.7 NEG
Anti Muscarinic Cholinergic Receptor 4 AB 2.3 NEG
Anti Muscarinic Cholinergic Receptor 5 AB 12.8 NEG
5/16/2017 and 5/17/2017: Dr. Kaufman tests: (4.5 weeks after infusion)
Parvo Virus B19 IgG 1.1 (<0.9) High (was negative in 2014)
Parvo Virus B19 IgM negative
Mycoplasma Pneumoniae IgG 1.81 (<0.9) High
Mycoplasma Pneumoniae IgM negative
Varicella Zoster Virus IgG 1100 (<135) High (down from 2014 a bit)
Varicella Zoster Virus IgM 1.87 (<0.9) High (up from 2014 a bit)
EBV Viral Capsid AG (VCA) AB IgG 2.65 (<0.9) High
EBV Viral Capsid AG (VCA) AB IgM negative
EBV Nuclear AG (EBNA) AB IgG 4.64 (<0.9) High
EBV DNA QN PCR <200 copies/mL
EBV Early Antigen D AB IgG 1.25 (<0.9) High
HSV 1 IgG 1.18 (<0.9) High (was negative in 2014)
HSV 2 IgG negative
HSV 1/2 IgM negative (was positive in 2014)
HHV6 IgG 1:80 (<1:10) High
HHV6 IgM negative
CMV IgG and IgM NEG
Chlamydophilia Pneumoniae AB IgG, IgM, IgA Not detected
Thyroglobulin Antibodies 3 (<1) High (was normal in 2014)
Thyroid Peroxidase Antibodies 4 (<9)
TSH 0.06 (0-4-4.5) Low
Free T4 0.6 (0.8-1.8) Low
Free T3 2.5 (2.3-4.2)
Vascular Endothelial Growth Factor (VEGF) <31 (31-86) Low
Lyme Blot: all non-reactive except 41 KD IgG and IgM bands
Anaplasma Phagocytophilum AB IgG, IgM NEG not detected
Ehrlichia Chaffeensis AB IgG, IgM NEG not detected
Bartonella Species AB w/reflex to titer
B. Henselae IgG, IgM NEG
B. Quintana IgG, IgM NEG
Babesia Microti IgG, IgM NEG not detected
SED Rate 6 (<20)
C-Reactive Protein <0.1 (5.4)
Vitamin D, 25-OH 61 (30-100)
Angioedema Panel
C1 Esterase Inhibitor, protein 24 (21-39)
Complement Component C1Q 6.4 (5.0-8.6)
C4D Fragment, EIA 2.0 (0.9-8.0)
Complement Component C4C 16 (16-47)
Myasthenia Gravis panel
Acetylcholine receptor binding antibody NEG
Acetylcholine receptor blocking antibody <15% binding inhibition NEG
Acetylcholine receptor modulating antibody <1% binding inhibition NEG
Rheumatoid Arthritis Diagnostic Panel 3
Rheumatoid Factor IgG, IgA, IgM all NEG
Cyclic Citrullinated Peptide (CCP) AB IgG NEG
Sjogren’s AB SS-A, SS-B NEG
ANA Multiplex w/reflex to 11 AB NEG
GAD65 (Glutamic Acid Decarboxylase 65) AB NEG
IA-2 AB NEG
Insulin Autoantibody NEG
Sensory Motor Neuropathy Antibody Panel (Ganglioside antobodies) all NEG
CMP — all within range
Urea Nitrogen 9
Creatinine 0.63
Sodium 141
Potassium 3.9
Chloride 108
Carbon dioxide 25
Calcium 9.0
Protein, total 6.2
Albumin 4.2
Globulin 2.0
Ratio 2.1
Bilirubin 0.5
Alkaline phosphatase 43
AST 14
ALT 16
CBC — all within range (hemoglobin almost low 11.7)
Lymphocyte Subset Panel 1 (CD3 CD4 CD8 CD16 CD56 CD19) all within range
IgG 805 (694-1618)
IgM 207 (48-271)
IgE 42 (<114)
IgA 96 (81-463)
Subclass 1 82 (46-378)
Subclass 2 31 (13-91)
Anti-IgA <16 (<99)
Anti-streptolysin O 110 (<200)
KIT D816 Mutation not detected
HLA-B27 Antigen NEG
Voltage Gated Calcium Channel (VGCC) AB Assay <30 NEG
Chromogranin A 9 (<15)
Tryptase 4 (<11)
Histamine <1.5 (0.1-1.8)
Prostaglandins PG D2, serum plasma 119 (35-115 pg/mL) High
Prostaglandins PG F2 Alpha 334 (80-240 pg/mL) High
06/18/2017: SIBO breath test, Dr. Kaufman: Very high

8/11/2017: Dr. B:
TSH <0.006 (0.45-4.50) Low
Free T4 0.64 (0.82-1.77) Low, but suppressed by T3 meds, so ok.
Free T3 4.3 (2.0-4.4)
10/16/2017: (Dr. I ordered by Dr. E) Day 10/11 of cycle, 14 days before period:
Testosterone 0.3 (0.0-0.8 ng/mL)
Testosterone, Free 2 (1-18 pg/mL)
Estradiol 282 (Periovulatory 95-433 pg/mL)
Progesterone 4.1 (Mid-Follicular 0.4-1.4 ng/mL; Mid-Cycle 0.6-2.0 ng/ml) High
DHEA Sulfate 130 (35-303 ug/dL)
Prolactin 16 (<25 ng/mL)
Sex Hormone Binding Globulin 144 (17-136) High
Ferritin 48 (10-180 ng/mL)
Iron, total 98 (31-171)
Iron binding capacity 346 (270-535)
Transferrin 247 (192-382)
Transferrin Saturation 28% (10-45%)
IgA 102 (84-499 mg/dL)
IgE 44 (0-214 [IU]/mL)
IgM 183 (40-350 mg/dL)
IgG 1,076 (610-1,616 mg/dL)
Subclass 1 672 (265-929 mg/dL)
Subclass 2 377 (200-550 mg/dL)
Subclass 3 17 (10-100 mg/dL)
Subclass 4 24 (4-86 mg/dL)
CBC — all within range (hematocrit almost low)
Lipid Panel
Cholesterol, Total 177 (<200 mg/dL)
Triglycerides 44 (39 mg/dL)
LDL 94 (<130 mg/dL)
Non-HDL Cholesterol 103 (0-159 mg/dL)
Cholesterol/HDL Ratio 2.4
10/24/2017: Dr. B:
Free T3 4.3 (2.0-4.4 pg/mL)
Free T4 0.45 (0.82-1.77 ng/dL) Low
TSH 0.006 (0.450-4.500 uIU/mL) Low
Thyroglobulin AB 16.3 (0.0 – 0.9 IU/mL) High (probably from IgG infusions)
TPO Auto AB 23 (0 – 34 IU/mL)
Estrogen, Total 306 (Day 19: 122 – 437 pg/mL)
11/13/2017: (Dr. I ordered by Dr. B): Candida Antibodies IgA 31 (0-9 U/mL) High
1/20/2018: Dr. B:
Free T3 5.0 (2.0-4.4 pg/mL) High
Free T4 0.49 (0.82-1.77 ng/dL) Low
TSH 0.015 (0.450-4.500 uIU/mL) Low
IGF-1 109 (118-298 ng/mL; Mean: 205) Low
1/31/2018: Dexa Bone Scan at Seattle Arthritis, ordered by Dr. B:
The scan shows loss at the femoral neck of your hip of 7.2% since 2014, this is concerning given the score is almost osteoporotic, your fracture risk remains low given your age, 5.8% at any site and 1.6% at the hip in the next 10 years.
4/20/2018: Dr. B:
Free T3 2.2 (2.0-4.4 pg/mL)
Free T4 0.29 (0.82-1.77 ng/dL) Low, but suppressed by T3, so ok.
TSH 0.018 (0.450-4.500 uIU/mL) Low
Vitamin D, 25, OH 48.5 (30.0-100.0 ng/mL)
6/5/2018: Dr. Kaufman tests (ordered by Dr. R): (3.5 weeks after 10g SCIG)
IgA 116 (84-499)
IgM 203 (40-350)
IgE 47 (0-214)
IgG
- Subclass 1 677 (265-929)
- Subclass 2 380 (200-550)
- Subclass 3 21 (10-100)
- Subclass 4 26 (4-86)
CMP — all within range
Urea Nitrogen 9
Creatinine 0.78
Sodium 135 (135-145)
Potassium 4.0
Chloride 104
Carbon dioxide 26
Anion Gap 5
Glucose 83
Calcium 9.3
Protein, total 6.4
Albumin 4.1
Bilirubin 0.5
Alkaline phosphatase 53
AST 17
ALT 22
CBC — all within range
Lymphocyte Subset Panel 1 (%CD3; abs CD3+; %CD4; abs CD4; %CD8; abs CD8; CD4/CD8 ratio) all within range (%CD8 almost high 35% (14-35%))
7/17/2018: Dr. Kaufman tests (ordered by Dr. R): (6 days after 2.5g IVIG)
- Baseline 24-hour urine tests (NOT during an episode; 3 days off of antihistamines):
- n-methylhistamine: 162 mcg/g Cr (30-200)
- prostaglandin D2 (PG D2): 27 ng/liter
- The Leukotriene E(4) and 2,3 Dinor 11 beta-prostagladin F2 Alpha concentrations in this sample was undetectable. Creatinine was also very low in the sample which may indicate a very dilute specimen. Repeat analysis is recommended.
- Creatinine conc: 17 mg/dL
Tryptase 4 (<11 ng/mL)
Histamine <1.5 (0.1-1.8)
Prostaglandins F2 Alpha 306 (80-240 pg/mL)
Prostaglandins PG D2, serum plasma 90 (35-115 pg/mL)
TSH 0.91 (0.4-4.5) Low
Free T4 0.3 (0.8-1.8) Low, but suppressed by T3 meds, so ok.
Free T3 2.5 (2.3-4.2)
9/7/2018: Dr. Broyles/Iller: Day 17, 15 days before next period (last day of follicular phase, day before ovulation, in theory):
Sex hormone binding globulin 108.3 (24.6-122.0 nmol/L)
Progesterone, plasma 3.3 ng/mL (Follicular phase 0.1-0.9; Ovulation 0.1-12.0)
DHEA 185 (41.2-243.7 ug/dL)
Testosterone, total 18 (8-48 ng/dL)
Testosterone, free 1.0 (0.0-4.2 pg/mL)
Estrogen fractionation, serum:
Estrone: 75 pg/mL (Follicular phase 39-132; Periovulatory 58-256)
Estradiol 122.9 pg/mL (Follicular phase 12.5-166.0; Ovulation phase 85.8-498.0)
Estrogen, total 492 pg/mL (11-20 Days 122-437) High
Vitamin D, 25-hydroxy 49.9 (30.0-100.0 ng/mL)
10/16/2018: Dr. Kaufman:
Creatinine concentration, urine 61 mg/dL
N-methylhistamine, urine 184 (30-200 mcg/g)
2,3 DINOR 11B PROSTAGLANDIN F2A,URINE 1939 (<5205 pg/mg)
LEUKOTRIENE E4, Urine 44 (</=104 pg/mg)
PROSTAGLANDIN D2 (PG D2), URINE Less than 20 ng/liter – Result is below the limit of quantitation.
Antiphospholipid Syndrome Panel: All negative.
Syndrome Early Sjogren’s Panel: All normal except CARBONIC ANHYDRASE VI IgG AB 82.9 EU/ml High
Lupus anticoagulant: not detected.
PTT-LA Screen 32 (</= 40 seconds)
Lymphocyte Subset Panel 1: All normal. CD3 (MATURE T CELLS – 85% Reference Range: 57-85%) and CD8 (SUPPRESSOR T CELLS – 42% Reference Range: 12-42%) at the very high end of normal.
12/20/2018: Dr. Broyles (day 19 of 38 day period, 19 days before next period, so follicular phase? Or luteal or ovulation, who knows):
TSH 0.994 (0.450-4.500 uIU/mL)
T4,free 0.50 (0.82-1.77 ng/dL)
T3,free 3.9 (2.0-4.4 pg/mL)
IGF-1 129 (118-298 ng/mL mean 205)
Estrogen fractionation, serum:
Estrone: 83 pg/mL (Follicular phase 39-132; Periovulatory 58-256)
Estradiol 87.2 pg/mL (Follicular phase 12.5-166.0; Ovulation phase 85.8-498.0)
Estrogen, total 166 pg/mL (11-20 Days 122-437; 21-30 Days 156-350)
02/08/2019: SIBO breath test, Dr. Kaufman: Very High

2/12/2019: Dr. Ryan: EKG: Normal sinus rhythm, Normal ECG
2/14/2019: Dr. Broyles: DEXA Bone Scan:
Normal spine L1-L4
Osteopenia hip
Osteoporosis femeral neck


2/14/2019: Dr. Ryan:
Ferritin 41 (10-180 ng/mL)
CBC: all normal
CMP: all normal, sodium, potassium, glucose (62) on the low side.
3/27/2019: Dr. Yak: 48-hour Holter monitor:
No significant pauses or AV Block noted. Normal PR, QRS, and QT intervals at varying heart rates. Maximum R-R interval is 1.37 seconds. Isolated APDs noted. No complex atrial arrhythmia. No ventricular arrhythmia noted. Diary submitted symptoms of “palpitations, flutter” correlated with isolated APDs.
Conclusions:
• Normal study showing sinus rhythm with rare premature atrial contractions.
• No arrhythmias detected.
• Normal sinus rhythm without ectopy during symptoms of “flutter.”
• Premature atrial contraction detected during two episodes of reported “palpitations.”
04/04/2019: Dr. Kaufman:
IgG total 1590 (694-1618 mg/dL)
IgG subclass 1 989 (382-929 mg/dL) High
IgG subclass 2 534 (241-700 mg/dL)
IgG subclass 3 37 (22-178 mg/dL)
IgG subclass 4 40.8 (4-86 mg/dL)
Chromogranin A 154 (25-140 ng/mL) High
Early Sjogren’s Panel: all normal except CARBONIC ANHYDRASE VI IgG AB 29.6 EU/ml High
EBV DNA, QN REAL TIME PCR <200 negative
CMV DNA, QN REAL TIME PCR <200 IU/mL negative
CMV DNA, QN PCR <2.30 IU/mL negative
HSV 1 and HSV 2 DNA, QN REAL TIME PCR <100 negative
HERPES VIRUS 6 DNA, RT REAL TIME PCR <500 negative
IgM 225 (48-271 mg/dL)
IgA 124 (81-463 mg/dL)
IgE 38 (</=114 kU/L)
LYMPHOCYTE SUBSET PANEL 1: all normal
4/4/2019: Dr. Yak: Echocardiogram:
There is mild aortic insufficiency. Mild aortic regurgitation is present. There is an eccentric jet of aortic insufficiency directed towards the septum. There is trace mitral regurgitation. Trace tricuspid regurgitation present.
4/4-5/4/2019: Dr. Yak : 30-day heart monitor:
The vast majority of episodes show normal sinus rhythm without ectopy. Some episodes of dizziness show sinus tachycardia. One PVC and one blocked PAC were observed.
04/10/2019: Dr. Kaufman:
T4, free 0.4 (0.8-1.8 ng/dL) Low
T3, free 3.9 (2.3-4.2 pg/mL)
TSH 0.78 (0.40-4.50 mIU/L)
Thyroglobulin AB 40 (</= 1 IU/mL) High
Thyroid Peroxidase AB 29 (<9 IU/mL) High
TRYPTASE 4 (<11 ng/mL)
HISTAMINE, PLASMA 1.5 (</= 1.8 ng/mL)
PROSTAGLANDINS F2 ALPHA (PGF2a) 94 (80-240 pg/mL)
PROSTAGLANDINS (PG D2), serum 86 (35-115 pg/mL)
04/15/2019: Dr. Kaufman:
VITAMIN B6 38.4 (2.1-21.7 ng/mL) High
VITAMIN K 1940 (80-1160 pg/mL) High
COPEPTIN 2 (</= 14 pmol/L)
VITAMIN A (RETINOL) 40 (38-98 mcg/dL)
ALPHA-TOCOPHEROL 10.5 (5.7-19.9 mg/L)
BETA-GAMMA-TOCOPHEROL <1.0 (5.4ng/mL)
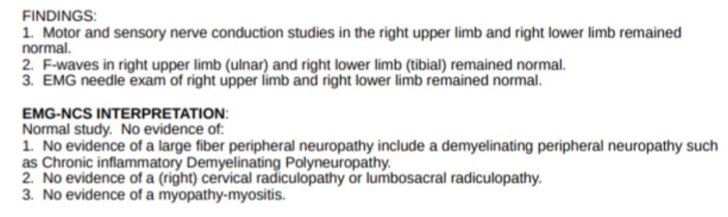
06/25/2019: EMG, sensory nerve conduction and motor nerve conduction studies, Dr. Gierke: Normal
07/17/2019: Dr. Ryan/Bolognese/Kaufman:
C-spine MRI: C4/5: Reversal of the normal cervical spine lordosis and shallow disc bulge at this level results in effacement of the ventral thecal sac and abutment of the ventral aspect of the cord.
Cine CSF flow MRI: There is attenuation of the dorsal CSF flow within the cerebral aqueduct.
07/18/2019: Dr. Broyles:
TSH 0.795 (0.450-4.500 uIU/mL)
T3, Free 2.2 (2.0-4.4 pg/mL)
T4, Free 0.4 (0.82-1.77 ng/dL)
Thyroglobulin AB 15.9 (0.0-0.9 IU/mL) High
Thyroid peroxidase (TPO) AB 27 (0-34 IU/mL)
08/09/2019: Therapath, Dr. Liou, ordered by Dr. Kaufman:
Small Fiber Neuropathy (SFN) Test (epidermal nerve fiber density test): Normal
Sweat Gland Nerve Fiber Density (SGNFD): no sweat glands found in thigh biopsy. Calf sample was normal: 55.0 (abnormal: < 36.5 low normal: 36.5 – 38.5)
08/21/2019: Sleep/ Wake EEG for brain symptoms, Dr. Gierke: Normal, read by the Epilepsy Center.
08/28/2019: Dr. Celmer:
Candida IgA 43 (0-9 u/mL) Very high — higher than it’s ever been.
DHEA 192 (<229 ug/dL)
09/21/2019: Dr. Celmer:
Candida IgG <10 (0-9 U/mL)
Candida IGM <30 (0-29 U/mL) Based on these 2 tests, Dr. C says I can stop Fluconazole and Diflucan. Keep taking 2 SF722s daily as maintenance.
10/17/19: Dr. Kaufman:
CBC: All normal
CMP: All normal except Potassium 3.3 (3.5-5.3 mmol/L) Low
Sodium 136 (135-146 mmol/L) and Creatinine 0.56 (0.50-1.10 mg/dL) were borderline low.
Free T3: 2.6 (2.3-4.2 pg/mL)
Free T4: 0.5 (0.8-1.8 ng/dL) Low
TSH: 0.06 (0.40-4.50 mIU/L) Low
Amino Acid Panel: All normal except:
ALPHA AMINOBUTYRIC ACID: 35 (7-32 umol/L) High
ETHANOLAMINE: 4 (5-13 umol/L) Low
Fatty Acid Panel:
MYRISTOLEIC, C14:1: 3.89 (4.65-32.47 umol/L) Low
HEXADECADIENOIC, C16:2: 5.10 (10.8-37.9 umol/L) Low
PALMITOLEIC, C16:1W7: 67.02 (68.5-570.2 umol/L) Low
MEAD, C20:3W9: 6.41 (10.3-41.3 umol/L) Low
PHYTANIC ACID: 3.37 (0.58-2.54 umol/L) High
Mannose Binding Lectin: 649 (NORMAL >=100 ng/mL)
Ferritin: 83 (16-232 ng/mL)
Total iron: 164 (40-190 mcg/dL)
Iron binding capacity: 312 (250-450 mcg/dL)
% Saturation: 53 (16-45 % (calc)) High
12/23/2019: Dr. Iller (3.5 days after IVIG):
EBV AB VCA IgG >600 (0.0-17.9) High
EBV AB VCA IgM negative
EBV Nuclear Antigen AB IgG 474 (0.0-17.9) High
EBV Early Antigen AB IgG 62.5 (0.0-8.9) High
Mycoplasma Pneumoniae IgG 505 (0-99) High
Mycoplasma Pneumoniae IgM negative
HHV6 IgG 6.38(<0.9) High
12/23/2019: Dr. Broyles (before taking thyroid meds, so almost 24 hours after last dose):
Free T3: 2.3 (2.0-4.4 pg/mL)
Free T4: 0.44 (0.82-1.77 ng/dL) Low
TSH: 0.337 (0.450-4.500 uIU/L) Low
12/27/2019: Dr. Bolognese/Li:
Kidney/bladder/renal/retroperitoneal ultrasound:
No evidence for urinary tract obstruction. Normal size and morphology, no hydronephrosis. Focal hypoechoic mass lower pole left kidney slightly larger than on the prior exam but still most consistent with an AML. Post void residual bladder volume 83.7 cc.
12/31/2019: Dr. Rampur:
Skin prick and intradermal allergy testing: Cefazolin, Lidocaine, Propofol, Rocuronium = neg
12/31/2019: Dr. Li/Bolognese:
Supine lumbar spine MRI:
- Conus ends at mid-L2. That is an automatic diagnosis of Tethered Cord, Classical variant.
- Vertical orientation of the cord
- Loss of lumbar lordosis
06/19/2020: Dr. Broyles/Li:
IGF-1: 100 (44-227); Z score 0.25 NEG T3: 2.7 (2.4-4.1 pg/mL) Free T4: 0.5 (0.6-1.2 ng/dL) Low TSH: 0.468 (0.400-5.000 uIU/L) CRP 0.5 (0.0-10.0 mg/L) SED rate 11 (0-20 mm/h) IgE, total 29 (0-214 [IU]/mL) IgA 138 (84-499 mg/dL) IgM 222 (40-350 mg/dL) IgG 1,941 (610-1,616 mg/dL) High DNase B Antibody Titer 146 (0-300 U/mL) Anti Streptolysin O Titer 200 (<100 [IU]/mL) High. This suggests you might have had a recent strep through infection. CBC Diff: all normal (WBC on the low end) CT ABDOMEN AND PELVIS: Peritoneum and Abdominal Wall: Mild mesenteric edema, nonspecific. Kidney: The 1.2 cm left lower pole hypodensity, unchanged compared to the CT from 2012, likely cyst. "It looks like there is a lot of stool in your intestines." All else unremarkable.
07/29/2020:
Left wrist and left middle finger fracture: Minimally displaced avulsion fracture at the ulnar aspect of the base of the distal phalanx of the middle finger. There is also a nondisplaced distal ulna fracture through the base of the styloid process.
09/26/2020: Dr. Li/Bolognese:
Prone lumbar MRI: Mild straightening. With prone positioning there is expected ventral displacement of the conus and cauda equina nerve roots. There is however persistent dorsal displacement of the filum terminale (series 1101, image 13) in relation to the structures without evidence of fatty filum. This finding raises concern for the possibility of occult tethered cord syndrome in the appropriate clinical scenario. Probable uterine fibroids measuring up to approximately 1 cm. Thoracic (supine) MRI: Scattered hemangiomas in marrow. Minimal disc protrusion at T7-T8. Otherwise, normal. Updated 09/26/2020








wow. looks like you’ve been a pin cushion. have you changed your diet since being found allergic to food items? has it helped?
LikeLike
For over a year I avoided legumes, dairy, gluten, eggs, tomatoes and all other nightshades, starchy veg, all grains except oats, all bad oils, and virtually all processed foods – nothing helped, not a thing, not at all. I guess I might be worse if I hadn’t changed my diet, but it’s pretty disheartening to feel absolutely no difference!
LikeLike
Man. I am so sorry. I can so empathize because for YEARS I knew something was wrong – but not until the brain tumor dx and Cowden’s Syndrome did anyone start to take my serious. I know you know this…but when those all came back “normal” (I’m looking at the thyroid stuff) did any doctor actually tell you your numbers? Meaning: maybe you’re borderline low/high and could benefit from therapy? I’m not trying to get in your biz and know this isn’t a cure all for your symptoms. I only clicked over here from another blog. I look forward to reading more. All the best.
LikeLike
I’m so tired of doctors and telling us to stop eating this and that. Those restrictive diets are really hard to stick to, especially when you’re sick already.
All those blood tests usually come back “normal” and docs say we are healthy. WRONG. Just not doing the right tests yet. Hopefully you do have a good doctor who is willing to journey through this with you but I also want to ask you, have you heard of the Fibromyalgia and Fatigue Centers http://www.fibroandfatigue.com/ Just throwing it out there to ya in case you wanted to try. I would if I could afford it!
LikeLike
AS for the fatigue the best and most natural option that has helped is ATP-20 supplements (www.douglaslabs.com about $20 for 60ct) and Glutathione/ATP injections which I get from my doctor for $10 each and I can’t afford that right now so I’ve been off them for a long while, but getting them once a week was helpful as far as energy only…not a huge difference when taking them, it’s a slight increase in energy, but once I had to give them up due to finances, I can sure feel the difference.
LikeLike
[…] the first two. Most everything on the methylation test was low (I’ve put the details in my tests page). He surmised that I had an MTHFR mutation (what I like to refer to as the “motherfucker […]
LikeLike
Do you have any luck with magnesium? I’ve been experimenting with magnesium malate, which has been show to help with fatigue, and find that, combined with fish oil and tryptophan I sleep much better. I love that you have such a detailed approach to this: it’s going to be such a great help to others facing the same–if not similar–challenges.
Also, how have you taken the glutathione? I’ve just tried to nebulise it but found it hurt my sinuses too much. I’m going to try less next time.
I’m sorry that you tried avoiding all those foods and didn’t find much difference. I’ve just come off an elimination diet and if I eat only certain things, I don’t get many gut symptoms but overall, it hasn’t improved my condition, which is totally annoying.
Anyway, good luck, and please keep sharing…
the world needs good role models! 🙂
LikeLike
[…] pretty much paleo diet (allowing rice), plus no eggs, citrus, nightshades or soy. I had a mycotoxin panel done and, in rare abnormal test results, found I had some very high levels in my urine. While […]
LikeLike
[…] put all my test results on this page. All of the MCAD urine tests were normal, which I expected, but was still frustrating. I am happy […]
LikeLike
[…] pillow, my sleep apnea oral appliance, my special food etc., I realised… No I don’t. My urine mycotoxin tests were high out of range. Eliminate all possible variables. Take nothing. Once I wrapped my head […]
LikeLike
[…] of test results (which can all be found here), I never mentioned the hormone panel and blood test results ordered by Dr. W in the last few […]
LikeLike
[…] only with coconut oil, nothing else. She’s hoping these will feed down both pathways to raise all the other hormones that are […]
LikeLike
Hi,
I wandered in looking for a low-sulfur, gluten-free left-over chicken and cilantro recipe and didn’t find it here, but Google must want me here for a reason.
Have you ever had a challenge heavy metals chelation test? Or have you checked other chemicals you might be carrying around that you shouldn’t be? The idea is that heavy metals and other toxins don’t necessarily stay in your blood, but end up in your bones, fat and organs. That would be sort of OK if they just sat there and didn’t do anything, and your body does its best to keep them that way, but when the level of toxins diminishes from your blood, the toxins leach back in again, and who knows what effects they might be having while incorporated into your bones and organs.
I have been listening to a bunch of webinars about detox, autoimmunity and thyroid since last summer – mostly interviews with functional/integrative medicine doctors, naturopaths, and a couple of pharmacists – and there seems to be a strong belief among that alternative community that a major reason for so many people with autoimmune conditions is toxins that end up attached to cells, causing the immune system to attack those cells. The thyroid might suck up some mercury and then the immune system attacks the thyroid, for example.
Then add a genetic tendency toward methylation problems, and you have more problems detoxifying yourself than other people. That’s why you get sick and they don’t. (Then again, some of those viruses you’ve been exposed to may be major factors. The changes that have been bred into wheat since the 1950s, along with a wheat-heavy diet full of extra gluten for fluffier bread is likely another factor for many of us.) The good news is that chelation therapy can get rid of mercury and lead, sweating can get rid of cadmium, and some foods and herbs are particularly good at helping you detoxify (like spirulina and cilantro, for example).
I’m glad to see that you are working with diet to help your CBS genes and methylation. But do check into toxins, because some people have had phenomenal results simply by detoxifying. Unfortunately, there are differences of opinion about how best to do that – some advocate lower levels of chelation for longer periods of time, which is less likely to shock the body, and some advocate careful testing to be sure to provide the right nutrient support while detoxifying strategies are going on. You need nutrients that help you make glutathione, but when you have sulfur issues it gets trickier.
I’m new to this myself and certainly don’t have the answers, but I thought it was worth raising the detox questions.
Best wishes for a dramatic recovery. I’m working on my own, but you have further to go.
LikeLike
get tesed for simian virus-40! was an Unknown contaminant of oral salk polio vaccine! ALSO, CHECK BLOOD LEVELS OF POLYCHLORINATED BIPHYNLS–PERSISTANT IN BODY FATS AFTER INGESTION–ARE ESTROGEN INTERRUPTORS. IN MY EXPERIENCE, EAT A MEDITERRANEAN DIET, DAILY MILD EXCERCISE, LITTLE COFFEE ANDALCOHOL. DUMP ALL RX AND FIND A DEDICATED ACCUPUNCTURIST!! MAY GOD BLESS YOU!!
LikeLike
[…] had a few blood tests done in January. The big shock is that my cholesterol is sky high. Total cholesterol is 310, LDL is […]
LikeLike
Elisabeth.
Your RealTime Labs Test shows 3 very Serious toxins
This your test results
11/13/2013: Mycotoxin urine test ~ Realtime labs:
Ochratoxin 5.25 (1.8-2.0) Positive
Aflatoxin 0.98 (0.8-1.0) Equivocal
Tricothecene 0.53 (0.18-0.2) Positive
This taken from real time labs site direct.
https://www.realtimelab.com/molds/
Which molds produce these mycotoxins?
Species Mycotoxin
Aspergillus Flavius Aflatoxin (AT)
A. ochraceus Ochratoxin A (OTA)
A. Niger OTA
Penicillium verrucosum OTA
Stachybotrys chartarum Macrocyclic Tricothecenes (MT)
A. versicolor Sterigmatocystin
A. fumigatus Gliotoxin
Chaetomium globosum Chaetoglobosin A, C
Fusarium sp. Simple Trichothecenes (e.g. T-2 and DON)
LikeLike
Elisabeth.
Your RealTime Labs Test shows 3 very Serious toxins
This your test results
11/13/2013: Mycotoxin urine test ~ Realtime labs:
Ochratoxin 5.25 (1.8-2.0) Positive
Aflatoxin 0.98 (0.8-1.0) Equivocal
Tricothecene 0.53 (0.18-0.2) Positive
This taken from real time labs site direct.
https://www.realtimelab.com/molds/
Which molds produce these mycotoxins?
Species……………………………..Mycotoxin
Aspergillus Flavius………………..Aflatoxin (AT)
A. ochraceus ……………………..Ochratoxin A (OTA)
A. Niger …………………………………….OTA
Penicillium verrucosum ……………….OTA
Stachybotrys chartarum …………….Macrocyclic Tricothecenes (MT)
A. versicolor …………………………Sterigmatocystin
A. fumigatus …………………………….Gliotoxin
Chaetomium globosum………………Chaetoglobosin A, C
Fusarium sp……………………Simple Trichothecenes (e.g. T-2 and DON)
LikeLike